Inflammatory Bowel Disease: Part I
Inflammatory bowel disease (IBD) includes two disorders: ulcerative colitis (idiopathic proctocolitis) and Crohn’s disease (regional enteritis). Both conditions are chronic and characterized by periods of exacerbation and remission. Although both diseases share many commonalities, each is distinctive in terms of its level, extent, and area of involvement. Exact etiology and pathogenesis are unknown, but a genetically associated autoimmune disorder activated by an infectious process is suspected. The changes produced by IBD result when immunocyte cells located in the mucosal layer are stimulated to release inflammatory mediators such as histamine, prostaglandins, leukotrienes, and cytokines. These act on the secretory and smooth muscle cells of the gastrointestinal tract, altering its functions and neuronal activity. Gastrointestinal salt and water transportation and the absorption and excretion of nutrients, salt, water, and electrolytes are affected. Onset of IBD occurs in late adolescence/young adulthood or around age 60. It occurs more commonly in whites than in African Americans or Asians, more commonly in Jewish than in non-Jewish persons, and more commonly in women than men. The incidence of ulcerative colitis is increased 40% among smokers. There is a familial component affecting approximately 10% of those with a first-degree relative who has IBD.
Ulcerative colitis is discussed here, and Crohn’s disease is discussed in Chapter 47.
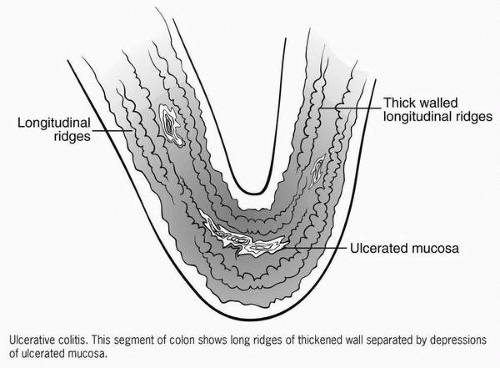 Figure 46-1 Ulcerative colitis.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|