Implanted Port Use
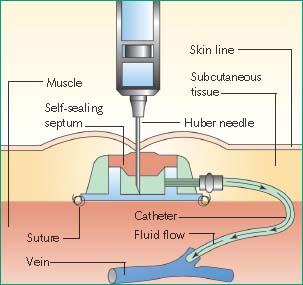
Surgically implanted under local anesthesia by a surgeon or interventional radiologist, an implanted port, also known as a vascular access device or a vascular access port, is a type of central venous access device. It consists of a silicone or polyurethane catheter attached to a reservoir, which is covered with a self-sealing silicone septum. The catheter is placed in the central venous system with the reservoir typically implanted in a subcutaneous pocket in the upper anterior chest wall. Alternatively, the reservoir may be placed in the upper arm, abdomen, side, or back.
An implanted port is used most commonly when some type of long-term IV therapy is required and an external central venous device isn’t appropriate or desirable. It can also be used to obtain blood samples for laboratory testing in these patients because they typically have limited vascular access. If the port isn’t adequately flushed after blood withdrawal, a thrombotic catheter occlusion can occur.
Nursing Alert
Limit blood sampling through the implanted port, when possible, to reduce the risk for central line–associated bloodstream infections.
An implanted port also may be used to administer a bolus injection or a continuous infusion of IV fluids, if necessary. Bolus injection requires only the time it takes to push the plunger of the syringe. Note, however, that many drugs have minimum and maximum injection rates, which must be timed.
Depending on patient needs, the type of port selected may have one or two lumens. A port can be used immediately after placement, although some edema and tenderness may persist for about 72 hours, making the device initially difficult to palpate and slightly uncomfortable for the patient. (See Understanding implanted ports.)
Once implanted, the port is accessed using a noncoring needle when IV therapy, catheter flushing, or blood withdrawal is required. This type of needle has a deflected point, which slices the port’s septum.
Only nurses who have been properly trained and validated may access and maintain implanted ports.1
Patients who require repeated computerized axial tomography scans with contrast may have a port implanted that has been specially developed to withstand the high pressures of power injectors. When using a power injector, a specialized access needle and tubing approved for power injection are required to ensure that the tubing and connections won’t rupture or separate.
Equipment
Assisting with Insertion
Noncoring needles (a noncoring needle has a deflected point, which slices the port’s septum) of appropriate type and gauge ▪ implanted port ▪ sterile gloves and gown ▪ mask ▪ cap ▪ antiseptic pads (alcohol, tincture of iodine, or chlorhexidine-based) ▪ chlorhexidine sponges ▪ extension tubing set, if needed ▪ local anesthetic (lidocaine without epinephrine) ▪ ice pack ▪ syringes prefilled with heparin and preservative-free normal saline flush solutions ▪ IV solution ▪ sterile dressings ▪ luer-lock injection cap ▪ clamp ▪ adhesive skin closures ▪ suture removal set ▪ insertion checklist.
Accessing A Top-Entry Port
Noncoring needle of appropriate type and gauge and attached extension set tubing ▪ gloves ▪ sterile gloves ▪ masks ▪ sterile drape ▪ 2% chlorhexidine applicator ▪ 10-mL syringes prefilled with preservative-free normal saline solution ▪ transparent semipermeable dressing ▪ injection or access cap ▪ catheter securement device, sterile tape, or sterile adhesive strips ▪ Optional: antiseptic soap, water, local anesthetic, ice pack, syringe prefilled with heparin flush solution (100 units/mL), ordered IV fluid, IV administration set, clippers, 2″ × 2″ sterile gauze dressing.
Some facilities use an implantable port access kit.
Obtaining A Blood Sample
Gloves ▪ appropriate antiseptic (alcohol, tincture of iodine, or chlorhexidine-based) ▪ prefilled flush syringes of preservative-free normal saline solution ▪ blood collection tubes ▪ laboratory request forms and labels ▪ laboratory biohazard transport bag ▪ Optional: protective eyewear or face mask, sterile injection cap, syringe prefilled with heparin flush solution.
For Vacutainer Method
Vacutainer with needleless adapter.
For Syringe Method
Blood transfer unit.
Administering A Bolus Injection
Patient’s medication administration record ▪ ordered medication in a syringe ▪ 10-mL syringes filled with preservative-free normal saline solution ▪ antiseptic pad (alcohol, tincture of iodine, or chlorhexidine-based) ▪ heparin flush (100 units/mL) ▪ Optional: port access equipment.
Preparation of Equipment
Assisting with Insertion
Confirm the size and type of the device and the insertion site with the doctor. Attach the tubing to the solution container and prime the tubing with fluid. Prime the noncoring needle with the extension set. All priming must be done using strict sterile technique, and all tubing must be free of air.2 After you’ve primed the tubing, recheck all connections for tightness. Make sure all open ends are covered with sealed caps.
Administering A Bolus Injection
Verify the order on the patient’s medication record by checking it against the doctor’s order.3,4 Know the actions, adverse effects, and administration rate of the medication to be injected.3
Perform hand hygiene and put on gloves.2,5,6,7 Avoid distractions and interruptions when preparing and administering medications to prevent medication errors.8 Visually inspect the solution for particulates, discoloration, or other loss of integrity and check the expiration date. If the integrity is compromised or the medication is expired, obtain a replacement from the pharmacy.4 If needed, draw up the prescribed medication in the syringe and dilute it, if necessary. Check the medication label three times while preparing it.4 Many medications come in unit-dose syringes.
Administering A Continuous Infusion
Review the patient’s medical record to determine the location of the implanted port and whether it’s currently accessed with a noncoring needle. If needed, access the port using the appropriate noncoring needle.
Understanding Implanted Ports
Typically, an implanted port is used to deliver intermittent infusions of medication, parenteral nutrition, chemotherapy, and blood products.17 Because the device is completely covered by the patient’s skin, the risk of extrinsic contamination is reduced. Patients may prefer this type of central line because it doesn’t alter the body image and requires less routine catheter care. The implanted port consists of a catheter connected to a small reservoir. A septum designed to withstand multiple punctures seals the reservoir. To access the port, a special noncoring needle is inserted perpendicular to the reservoir.
 |
Implementation
Assisting with Insertion
Conduct a preprocedure verification to make sure that all relevant documentation, related information, and equipment are available and correctly identified to the patient’s identifiers.9
Check the patient’s history for hypersensitivity to local anesthetics or chlorhexidine.
Although the doctor is responsible for obtaining consent for the procedure, make sure the written document is signed, witnessed, and in the patient’s medical record.10,11
Use an insertion checklist to adhere to infection prevention and safety practices during insertion. Stop the procedure immediately if you observe any breaks in sterile technique.
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.13
Reinforce to the patient the doctor’s explanation of the procedure, its benefit and risks, and what’s expected of the patient during and after implantation.
Allay the patient’s fears and answer questions about movement restrictions, cosmetic concerns, and management regimens.
Put on the mask, cap, sterile gloves, and gown.2
Conduct a time-out immediately before starting the procedure to determine that the correct patient, site, positioning, and procedure are identified, and confirm, as applicable, that relevant information and necessary equipment are available.14 The doctor will surgically implant the port, most likely using a local anesthetic. Occasionally, however, a patient may receive a general anesthetic.
The insertion site is prepared using a chlorhexidine-based antiseptic and allowed to dry.
During the procedure, you may be responsible for handing equipment and supplies to the doctor.
After draping the patient from head to toe to comply with maximal barrier precautions,2 the doctor makes a small incision and introduces the catheter, typically into the superior vena cava through the subclavian, jugular, or cephalic vein. After fluoroscopy verifies correct placement of the catheter tip, the doctor creates a subcutaneous pocket over a bony prominence in the chest wall. Then he tunnels the catheter to the pocket. Next, he connects
the catheter to the reservoir, places the reservoir in the pocket, and flushes it with heparin solution. Lastly, he sutures the reservoir to the underlying fascia and closes the incision.
Apply a sterile occlusive dressing.
Dispose of used equipment and discard of waste in the appropriate receptacle.
Accessing A Top-Entry Port
Verify the doctor’s order for obtaining access.
Check the patient’s record for allergies.
Gather the necessary supplies.
Confirm the patient’s identity using at least two patient identifiers according to your facility’s policy.13
Explain the procedure to the patient and answer any questions to decrease his anxiety and promote his cooperation.
If ordered, apply a topical anesthetic to reduce the pain associated with the needle insertion. Depending on the anesthetic used, the time for effective anesthesia may vary from a few minutes to 1 hour. Alternatively, place an ice pack over the area for several minutes to alleviate possible discomfort from the needle puncture.
Place the patient in a reclining position or in a chair with a pillow behind his shoulder.
Find the port location and assess for any signs of inflammation (redness, swelling, or induration) or skin breakdown. If present, report your findings to the doctor.
If excessive hair is present, clip it.18
If the site is visibly soiled, wash it with antiseptic soap and water.
Open the supplies, and prepare a sterile field using a sterile drape. Using sterile technique, place the supplies on the sterile field.
Put on a mask (according to your facility’s policy) and sterile gloves and wear them throughout the procedure.1
Prepare the noncoring needle by attaching a 10-mL syringe of sterile preservative-free normal saline solution and priming the extension set and needle.
Clean the area with the 2% chlorhexidine applicator, using a back-and-forth scrubbing motion, and allow the area to dry.2,18
Remove and discard your gloves and perform hand hygiene.5,6,7,12 Put on a new pair of sterile gloves.
Palpate the area over the port to find the port septum.
Anchor the port with your nondominant hand. Then, using your dominant hand, aim the needle at the center of the device.
Insert the needle perpendicularly to the port septum. Push the needle through the skin and septum until you reach the bottom of the reservoir.
Check needle placement by aspirating for blood return.1
If you can’t obtain blood, remove the needle and repeat the procedure. Ask the patient to raise his arms and perform Valsalva’s maneuver. If you still don’t get blood return, notify the doctor; a fibrin sleeve on the distal end of the catheter may be occluding the opening. (See Managing implanted port problems.)
Flush the device with preservative-free normal saline solution. If you detect swelling or if the patient reports pain at the site, remove the needle and notify the doctor.
Secure the needle using a catheter securement device, sterile tape, or sterile adhesive strips. If necessary, place a folded 2″ × 2″ sterile gauze pad underneath the wings of the access needle without obscuring the insertion site to prevent the needle from rocking within the septum.
Cover the site with a transparent semipermeable dressing or gauze dressing.
Attach the end of the extension tubing to an IV infusion. If a continuous infusion isn’t ordered, instill 3 mL of heparin (100 units/mL) to heparin-lock the device.19 You may also attach an injection or access cap to the tubing if no infusion is being administered at this time.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
