Hyperparathyroidism
Characterized by overactivity of one or more of the four parathyroid glands, hyperparathyroidism results in excessive secretion of parathyroid hormone (PTH). Increased PTH levels act directly on the bone and kidney tubules, causing an increase of calcium in the extracellular fluid that can’t be compensated for by renal excretion or uptake into the soft tissues
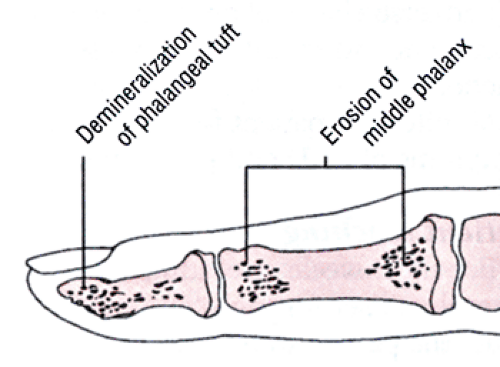
or skeleton. (See Bone resorption in primary hyperparathyroidism.)
or skeleton. (See Bone resorption in primary hyperparathyroidism.)
Hyperparathyroidism is most common in females (especially those who are postmenopausal), with onset usually occurring between the ages of 35 and 65. The disorder is classified as primary or secondary, based on its cause.
Causes
In primary hyperparathyroidism, one or more of the parathyroid glands enlarges, increasing PTH secretion and elevating serum calcium levels. The cause of primary hyperparathyroidism is unknown. A genetic factor may be involved. Also, patients with thyroid carcinoma who have had neck irradiation have developed primary hyperparathyroidism.
In secondary hyperparathyroidism, excessive compensatory production of PTH stems from a hypocalcemia–producing abnormality outside the parathyroid gland, which causes a resistance to the metabolic action of PTH. Rickets, chronic renal failure, vitamin D deficiency, osteomalacia due to laxative abuse or phenytoin use, or an excessive intake of thiazide diuretics, vitamin D, or calcium supplements may cause hypocalcemia.
Complications
Untreated hyperparathyroidism damages the skeleton and kidneys from hypercalcemia. Bone and articular problems—such as chondrocalcinosis; occasional severe osteopenia, especially of the vertebrae; erosions of the juxta–articular surface; subchondrial fractures; traumatic synovitis; and pseudogout—may occur. Renal complications include renal calculi, renal colic, nephrolithiasis, urinary tract infections, renal insufficiency and, eventually, renal failure.
Other possible complications include peptic ulcers, cholelithiasis, pancreatitis, cardiac arrhythmias, vascular damage, hypertension, and heart failure. Severe hypercalcemia may cause parathyroid poisoning, which includes central nervous system (CNS) changes, renal failure, rapid precipitation of calcium throughout the soft tissues and, possibly, coma.
Assessment
The clinical effects of primary hyperparathyroidism result from hypercalcemia and are typically present in several body systems:
renal—nephrocalcinosis due to elevated levels of calcium and, possibly, recurring nephrolithiasis, which may lead to renal insufficiency. Renal manifestations, including polyuria, are the most common effects of hyperparathyroidism.
skeletal and articular—chronic lower back pain and easy fracturing due to chondrocalcinosis; osteopenia and osteoporosis, especially on the vertebrae; erosions of the juxta–articular surface; subchondral fractures; traumatic synovitis; and pseudogout.