H
HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 went into effect in the spring of 2003 to strengthen and protect patient privacy. Health care providers (such as doctors, nurses, pharmacies, hospitals, clinics, and nursing homes), health insurance plans, and government programs (such as Medicare and Medicaid) must notify patients about their right to privacy and how their health information will be used and shared. This includes information in the patient’s medical record, conversations about the patient’s care between health care providers, billing information, health insurers’ computerized records, and other health information. Employees must also be taught about privacy procedures.
Under HIPAA, the patient also has the right to access his medical information, know when health information is shared, and make changes or corrections to his medical record. Patients also have the right to decide if they want to allow their information to be used for certain purposes, such as marketing or research. Patient records with identifiable health information must be secured so that the records aren’t accessible to those who don’t have a need for them. Identifiable health information may include the patient’s name, Social Security number, identification number, birth date, admission and discharge dates, and health history.
When a patient receives health care, he will need to sign an authorization form before protected health information can be used for purposes
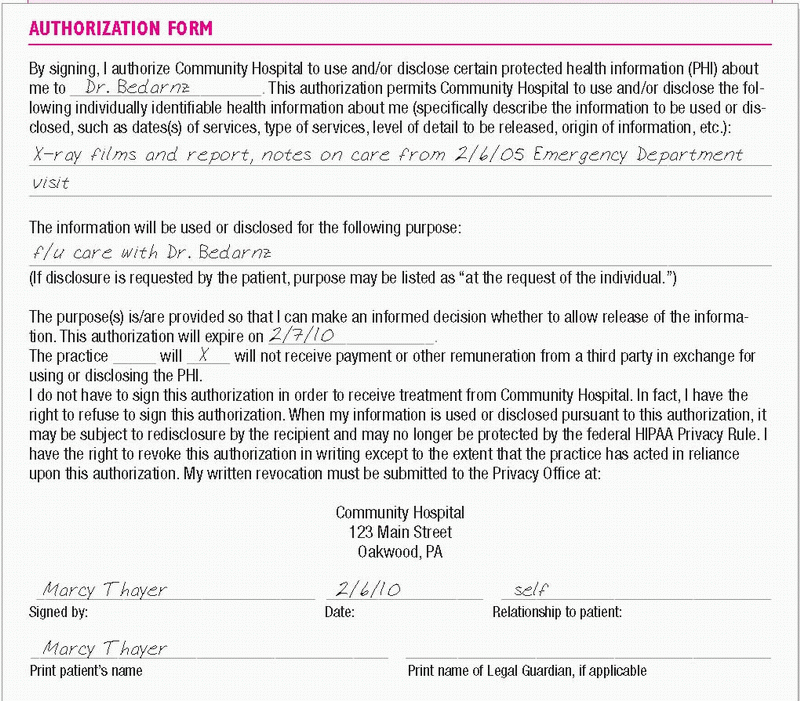
other than routine treatment or billing. The form should be placed in the patient’s medical record. (See Documenting patient authorization to use personal health information.)
other than routine treatment or billing. The form should be placed in the patient’s medical record. (See Documenting patient authorization to use personal health information.)
 DOCUMENTING PATIENT AUTHORIZATION TO USE PERSONAL HEALTH INFORMATION
DOCUMENTING PATIENT AUTHORIZATION TO USE PERSONAL HEALTH INFORMATIONYour agency probably has an authorization form similar to the one below to be used for release of a patient’s personal health information for reasons other than routine treatment or billing. Make sure all the required information is completed before having the patient or legal guardian sign the form.
|
ESSENTIAL DOCUMENTATION
Use your agency’s HIPAA authorization form to document your patient’s consent for the use and disclosure of protected health information. An authorization form must include a description of the health information that will be used and disclosed, the person authorized to use or disclose the information, the person to whom the disclosure will be made, an expiration date, and the purpose for sharing or using the information. The form is to be signed by the patient or legal guardian and placed in the patient’s medical record.
HEARING IMPAIRMENT
Hearing loss occurs in varying degrees that range from the loss of only certain tones to total deafness. Hearing loss is most commonly classified by the cause of the impairment. Conductive loss results from the failure of sound waves to be transmitted through the external ear, middle ear, or both. Sensorineural loss results from pathologic changes in the inner ear, 8th cranial nerve, auditory centers of the brain, or all three. Mixed loss is a combination of conductive and sensorineural loss. Central hearing loss is a result of damage to the brain’s auditory pathways or auditory center. Gross or precise assessment can be done to determine the extent of the hearing loss.
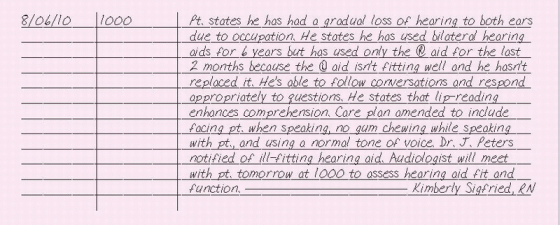
ESSENTIAL DOCUMENTATION
Determine the length of time that your patient has had the hearing loss. Describe the patient’s degree of hearing loss and whether it’s unilateral or bilateral. Note if the increased hearing loss is more significant in one ear. Record whether any hearing aids are being used. Include the effectiveness of hearing aids and the use of secondary modes of communication. Determine what additional methods are currently being used to compensate for the loss, such as lip-reading, sign language, picture boards, or writing pads. Update the nursing care plan to reflect alternative forms of communication with your patient.
|
HEART FAILURE, DAILY ASSESSMENT
A syndrome characterized by myocardial dysfunction, heart failure leads to impaired pump performance (reduced cardiac output) or to frank heart failure and abnormal circulatory congestion. Congestion of systemic venous circulation in right-sided heart failure may result in peripheral edema or hepatomegaly; congestion of pulmonary circulation in left-sided heart failure may cause pulmonary edema, an acute, life-threatening emergency.
Although heart failure may be acute (as a direct result of myocardial infarction), it’s generally a chronic disorder associated with the retention of sodium and water by the kidneys. Care for a patient with heart failure centers on symptom management, fluid balance, and prevention and management of complications.
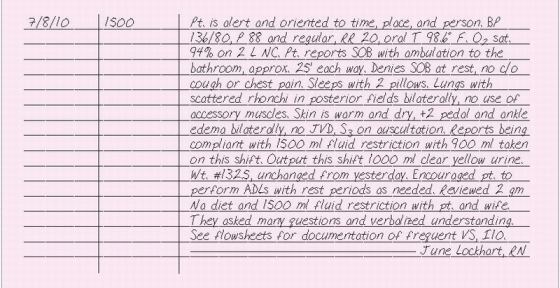
ESSENTIAL DOCUMENTATION
Record the date and time of your entry. Record your patient’s subjective symptoms, such as shortness of breath, cough, activity intolerance, chest pain, orthopnea, and fatigue. Document your assessment of the respiratory system (adventitious breath sounds, use of accessory muscles, respiratory rate, pulse oximetry, and signs and symptoms of hypoxia) and cardiovascular system (jugular vein distention, abnormal heart sounds, heart rate, blood pressure, pallor, diaphoresis, cool, clammy skin, hemodynamic monitoring results, cardiac rhythm, the degree and location of edema, urine output, and mental status). Include any new laboratory data, ECG findings, and chest X-rays.
Record interventions, such as daily weight measurements, fluid restriction, I.V. therapy, and oxygen therapy, and the patient’s response. Chart drugs given during your shift on the medication administration record or medication Kardex. Daily intake and output are recorded on the intake and output record. (See “Intake and output,” pages 216 to 218.) Record patient education on such topics as energy conservation, disease process, nutrition, fluid restrictions, daily weights, drugs and other treatments, and signs and symptoms to report to the nurse or doctor. Some facilities may use a patient education record to document any teaching you provide (See “Patient teaching,” pages 293 to 298.)
|
HEAT THERAPY
Heat therapy is warmth applied directly to the patient’s body that raises tissue temperature and enhances the inflammatory process by causing vasodilation and increasing local circulation. This promotes leukocytosis, suppuration, drainage, and healing. Heat therapy also increases tissue metabolism, reduces pain caused by muscle spasm, and decreases congestion in deep visceral organs. Moist heat softens crusts and exudates and penetrates deeper than dry heat.
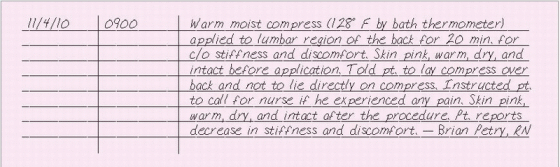
ESSENTIAL DOCUMENTATION
Record the date and time of the application; the reason for the use of heat; the site of application; the type of heat used, such as dry or moist; the type of device, such as a hot-water bottle, electric heating pad, K pad,
chemical hot pack, or warm compresses; the temperature or heat setting; measures taken to protect the patient’s skin; and the duration of time the heat was applied. Include the condition of the skin before and after the application of heat therapy, signs of complications, and the patient’s response to the treatment. Record any patient education provided.
chemical hot pack, or warm compresses; the temperature or heat setting; measures taken to protect the patient’s skin; and the duration of time the heat was applied. Include the condition of the skin before and after the application of heat therapy, signs of complications, and the patient’s response to the treatment. Record any patient education provided.
|
HEMODYNAMIC MONITORING
Continuous pulmonary artery pressure (PAP) and intermittent pulmonary artery wedge pressure (PAWP) measurements provide important information about left ventricular function and preload. This information is useful not only for monitoring, but also for aiding diagnosis, refining your assessment, guiding interventions, and projecting patient outcomes.
Nearly all acutely ill patients are candidates for PAP monitoring—especially those who are hemodynamically unstable, who need fluid management or continuous cardiopulmonary assessment, or who are receiving multiple or frequently administered cardioactive drugs. PAP monitoring is also crucial for patients with shock, trauma, pulmonary or cardiac disease, or multiorgan disease. It’s also used before some major surgeries to obtain baseline measurements.
Current pulmonary artery (PA) catheters have up to six lumens. In addition to distal and proximal lumens used to measure pressures, a balloon inflation lumen inflates a balloon for PAWP measurement and a thermistor connector lumen allows cardiac output measurement. Some catheters also have a pacemaker wire lumen that provides a port for pacemaker electrodes and measures continuous mixed venous oxygen saturation.
The PA catheter is inserted into the heart’s right side with the distal tip lying in the pulmonary artery. Fluoroscopy may not be required during catheter insertion because the catheter is flow directed, following venous blood flow from the right heart chambers into the pulmonary artery.
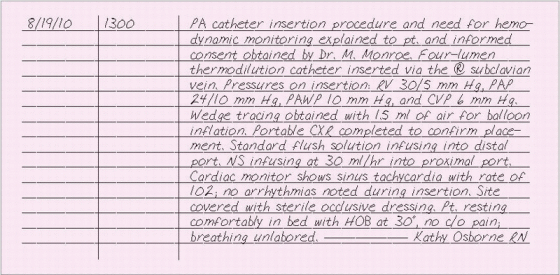
ESSENTIAL DOCUMENTATION
Document the date and time of catheter insertion. Include the name of the doctor who performed the procedure. Identify the number of catheter lumens, catheter insertion site, the pressure waveforms and values of the various heart chambers, and the balloon inflation volume required to obtain a wedge tracing. Note whether any arrhythmias occurred during or after the procedure. Document any solution infusing through the catheter ports. Record the type of flush solution used and its heparin concentration (if any). Describe the type of dressing applied and the patient’s tolerance of the procedure. Chart all site care, dressing changes, tubing, and solution changes.
|
HOME CARE, HOME CARE AIDE NEEDS
Home care aides provide hands-on personal care to the patient or services needed to maintain the patient’s health or facilitate his medical treatment. Aides also provide respite to caregivers. Remember that Medicare will reimburse only for care provided by a certified level III home care aide.
You’re responsible for developing the aide’s care plan and supervising her activities in the patient’s home. Most agencies use a standard care plan or duty assignment sheet for this purpose that can be adapted to fit each patient’s needs.
To maintain state licensure and certification from Medicare and the Joint Commission, your agency must require the home care aide to follow the patient’s care plan and to complete a separate home care aide note or entry in the patient’s clinical record for every visit.
ESSENTIAL DOCUMENTATION
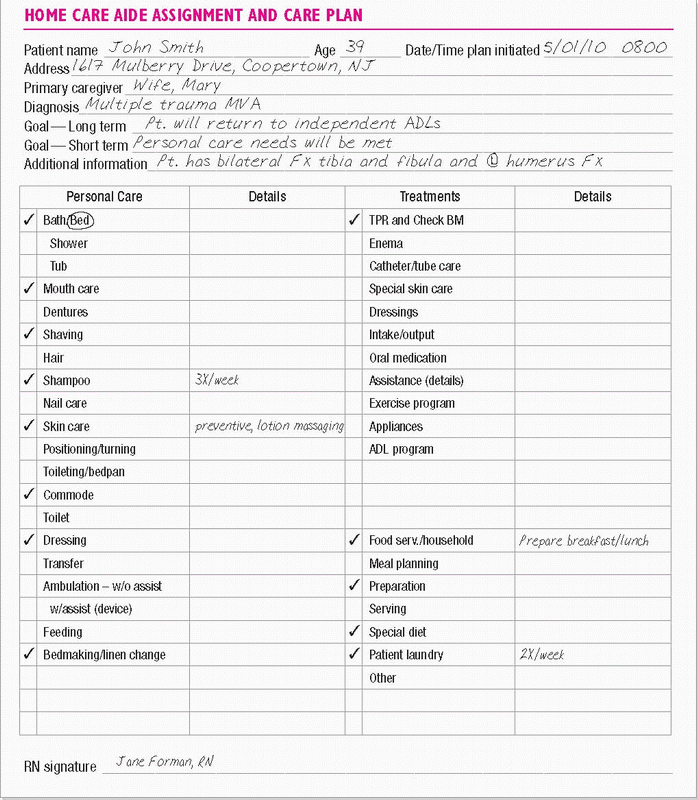
On the home care aide assignment and care plan form, you must itemize every activity that the aide is permitted to provide. This form may consist of a checklist of services and should include the date and time that the plan was initiated. (See Home care aide assignment care plan, page 165.) If the care plan was revised, this date and time must also be included. The patient’s name, identifying information, doctor’s name, diagnosis, and short- and long-term goals are also included on the plan.
HOME CARE, INITIAL ASSESSMENT
After you have received a referral and orders to begin home care, you need to perform a thorough assessment of the patient and his home environment to set reasonable goals and tailor the care to the patient’s specific needs. Assessments vary slightly from agency to agency, but the basic information required for completion is the same.
The proposed Conditions of Participation for Home Health Agencies requires that Medicare-certified agencies complete a comprehensive assessment of home care patients using a standardized data set called the Outcome and Assessment Information Set (OASIS). OASIS was developed specifically to measure outcomes for adults who receive home care. Using this instrument, you’ll collect data to measure changes in your patient’s health status over time. Typically, you’ll need to collect OASIS data when a patient starts home care, at the 60-day recertification point, and when the patient is discharged or transferred to another health care facility, such as a hospital or subacute care facility. (See OASIS — Be careful how you chart.)
ESSENTIAL DOCUMENTATION
Use your agency’s form to thoroughly and specifically document your assessment of the patient’s:
nutritional status
home environment in relation to safety and supportive services and groups, such as family, neighbors, and community
knowledge of his disease or current condition, prognosis, and treatment plan
potential for complying with the treatment plan.
When completing the OASIS data set, you’ll fill in or check off information on more than 80 topics, including:
sociodemographic data
physiologic data
functional data
service utilization data
mental, behavioral, and emotional data.
OASIS—BE CAREFUL HOWYOU CHART
The Outcome and Assessment Information Set (OASIS) was first implemented in 1999 to measure outcomes in home health care. In October of 2000, the OASIS format changed because of the new Medicare payment system for home health care called Prospective Payment System (PPS). What you document can have a significant impact on services your patient receives and the reimbursement your agency collects. The OASIS format was revised again in October 2007 to simplify certification extensions, expand therapy visits, and increase the number of diagnoses that will be a case mix diagnosis.
A point system is established for certain questions on the OASIS form, and it determines the reimbursement your agency will receive. For example, if your patient has had coronary artery bypass graft surgery and has two wounds, you must document each wound in the appropriate sections of the OASIS form. Failure to document one or both of the wounds could potentially cost your agency a significant amount of money.Wounds are just one of the indicators that govern how much your agency will be reimbursed for patient care.
Problems can also occur when your assessment on the OASIS form is inconsistent with the doctor’s orders. For example, if the doctor has ordered gait training and transfers but you document on the OASIS form that your patient can transfer and ambulate independently, the entire claim may be denied because physical therapy isn’t needed if the patient is independent.
These OASIS tools will be used by Medicare to compare information and review claims. If you have any questions about how to correctly answer OASIS questions in a given circumstance, contact your supervisor or continuous quality improvement nurse. Keep in mind that what you document has significant impact on your patient and your agency. Read the questions carefully and be sure of your answers.You do make a difference!
HOME CARE, INTERDISCIPLINARY COMMUNICATION IN
Communication between members of the home health care team is essential when caring for a patient at home. Ideally, the team works together toward similar goals to help the patient reach the expected outcomes. Agencies accomplish interdisciplinary communication in various ways. During patient care conferences, the team discusses the patient’s care plan and any changes needed in treatment. Between these conferences, team members may communicate with one another through voice mail systems. However, the most important form of interdisciplinary communication is the agency’s interdisciplinary communication form. Surveyors place a great deal of emphasis on this form, which shows when, why, and by whom a care plan was changed. It clearly defines deviations from the original care plan. Because the information documented on this form becomes part of the legal chart, follow the guidelines for accurate documentation.
ESSENTIAL DOCUMENTATION
When completing an interdisciplinary communication form, be sure to fill in the following:
patient’s name and identification number
date and time
your name and title
name and title of the person to whom you’re giving or from whom you’re receiving the information
subject matter discussed (for example, abnormal laboratory results)
changes to the care plan as a result of this communication
name of team members notified of the change in the care plan
outcome of the conversation and any agreements made
actions you took
your signature and title.
When you speak to another member of the home health care team by phone or voice mail message, the same basic information should be documented.
See Interdisciplinary communication form for sample documentation.
 INTERDISCIPLINARY COMMUNICATION FORM
INTERDISCIPLINARY COMMUNICATION FORMStay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access

 HOME CARE AIDE ASSIGNMENT CARE PLAN
HOME CARE AIDE ASSIGNMENT CARE PLAN