Gastrointestinal Disorders
QUICK LOOK AT THE CHAPTER AHEAD
The four common disorders in the gastrointestinal (GI) system are motility, inflammatory, structural, and obstructive. Complications related to these include malabsorption, fluid and electrolyte disturbances, malnutrition, and poor growth. Examples of each of the four disorders are discussed.
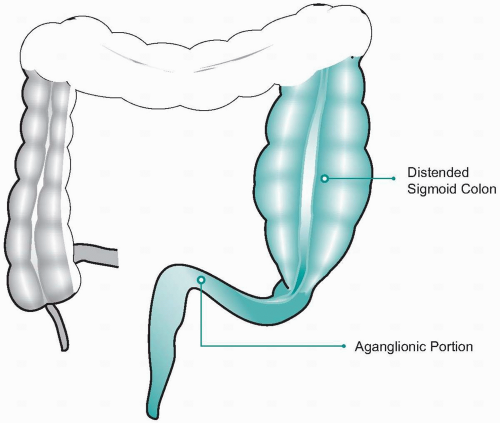
Pyloric stenosis is the most common upper GI disorder requiring surgery during the neonatal period (Figure 32-1). It is often seen in male infants between the ages of 1 and 6 months. It is common in first-born white males, less common among African-Americans, and rare in Asians. Increased gastrin secretion in the last trimester by the mother has been found to increase the chance of having pyloric stenosis.
Pathophysiology
Pyloric stenosis, an example of an obstructive disorder, occurs when the muscle at the pylorus narrows and thickens due to an increase in cell size and cell number. Hypertrophy and hyperplasia cause the circular muscle
of the pylorus to thicken. Swelling and inflammation reduce the opening and could result in complete obstruction.
of the pylorus to thicken. Swelling and inflammation reduce the opening and could result in complete obstruction.
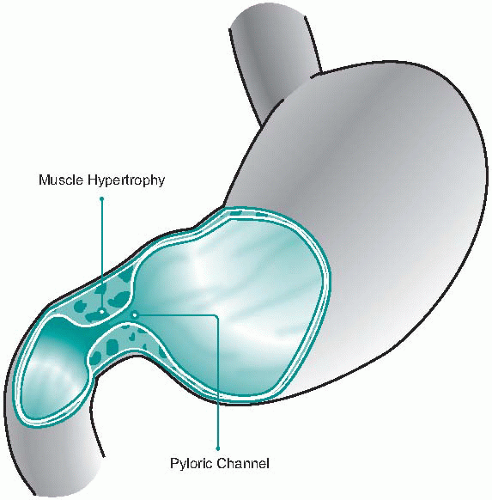 Figure 32-1 Pyloric stenosis. |
The cardinal finding in pyloric stenosis is often an olive-sized bulge below the right costal margin. It can be easily palpated when the infant is relaxed and has an empty stomach. Other significant symptoms include projective vomiting during or shortly after feedings, constipation, poor weight gain, and often dehydration and lethargy as the symptoms progress. If undetected, severe fluid and electrolyte imbalances can occur, such as metabolic alkalosis, often leading to chronic malnutrition and fatalities.
Treatment
Pyloric stenosis is treated by intravenous therapy to correct the electrolyte imbalances, nothing by mouth before surgery, and surgical treatment, called a pyloromyotomy, in which the muscles are split and separated. Feedings are usually begun 4-6 hours after surgery, and the procedure has a high success rate.
Hirschsprung’s disease is a motility disorder that commonly coexists with other congenital anomalies, particularly Down’s syndrome (Figure 32-2). It is four times more common in males and accounts for about one fourth of all cases of neonatal obstruction.
Pathophysiology
Hirschsprung’s disease, also called congenital aganglionic megacolon, results from an absence of ganglion cells in one or more segments of the colon. The aganglionic segment is narrowed, with a dilated portion of the proximal normal colon. Lack of enervation causes peristalsis, and stool accumulates in the distal portion of the colon, resulting in obstruction. As
a result, findings include liquid or ribbon-like stool, distended abdomen, signs of dehydration, and often enterocolitis, inflammation of the small intestine and colon. In the newborn period, the newborn may fail to pass meconium within 24 to 48 hours after birth. A rectal biopsy confirms diagnosis by showing the absence of ganglionic cells.
a result, findings include liquid or ribbon-like stool, distended abdomen, signs of dehydration, and often enterocolitis, inflammation of the small intestine and colon. In the newborn period, the newborn may fail to pass meconium within 24 to 48 hours after birth. A rectal biopsy confirms diagnosis by showing the absence of ganglionic cells.
Treatment
Surgical resection of the aganglionic segment is the treatment of choice and is usually delayed until the child is around 6 months old. Initially, a colostomy may be created proximal to the aganglionic section to relieve obstruction. This allows the child to gain weight, gives the bowel a rest, and provides a means for the child to defecate. A second procedure would reverse the colostomy and resect or remove the involved area. This procedure
is performed when the child is between 6 and 15 months of age or weighs between 18 and 20 pounds.
is performed when the child is between 6 and 15 months of age or weighs between 18 and 20 pounds.
Intussusception is the most frequent cause of intestinal obstruction in the first 2 years of life, peaking between the third and ninth month of life (Figure 32-3). It is twice as common in males as females, and in most cases the cause is unknown.
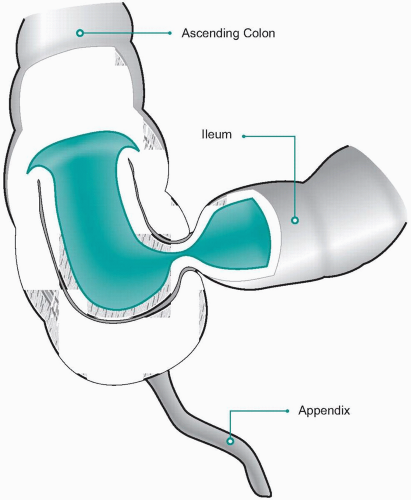 Figure 32-3 Intussusception. |
Pathophysiology
Intussusception occurs in the lower gastrointestinal tract as one segment of the bowel telescopes into the lumen of the adjacent section of intestine. The walls of the bowel press against each other, become inflamed and edematous, and may cause bleeding. A cardinal sign in about one half of infants is current jelly-like stools caused by blood and mucus in the stool. As it progresses, abdominal distention and vomiting occur, eventually leading to necrosis and perforation if left untreated. The infant may appear lethargic and listless with risk of weak thready pulse, shallow respirations, and a marked elevation in temperature.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree