Gastric Cancer
Although gastric cancer is common throughout the world in people of all races, its incidence exhibits unexplained geographic, cultural, and gender differences. For example, mortality from this disorder is high in Japan, Iceland, Chile, and Austria. Incidence is also higher in males older than age 40.
Over the past 25 years in the United States, the incidence of gastric cancer has fallen 50%, with the resulting death rate now one-third of what it was 30 years ago. This decrease has been attributed, without proof, to the improved, well-balanced diets most Americans enjoy. Aspirin and other nonsteroidal anti-inflammatory drugs may also play a role in preventing the occurrence of gastric cancer.
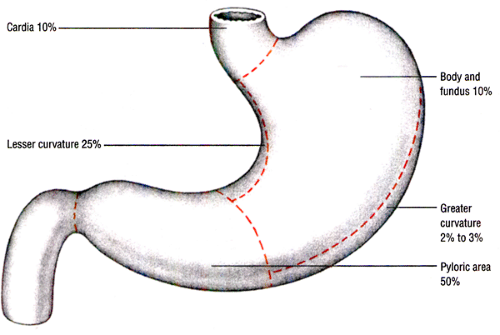
Gastric cancer occurs more commonly in some parts of the stomach than in others. (See Sites of gastric cancer.)
This adenocarcinoma rapidly infiltrates the regional lymph nodes, omentum, liver, and lungs by way of the walls of the stomach, duodenum, and esophagus; the lymphatic system; adjacent organs; the bloodstream; and the peritoneal cavity.
The patient’s prognosis depends on the stage of the disease at the time of diagnosis. Overall, the 5-year survival rate is about 15%.
Causes
The cause of gastric cancer is unknown; however, predisposing factors such as gastritis with gastric atrophy are known to increase the risk. Genetic factors have also been implicated. People with type A blood have a 10% increased risk, and the disease occurs more commonly in people with a family history of such cancer.
Dietary factors related to food preparation and preservation, such as smoked foods, pickled vegetables, and salted fish and meat, may also be implicated. Furthermore, excessive alcohol consumption and smoking increase the risk of developing gastric cancer.
Complications
Malnutrition occurs when the stomach can’t digest protein, and GI obstruction develops as the tumor enlarges. Iron deficiency anemia results as the tumor causes ulceration and bleeding. If the patient has pernicious anemia, the tumor can interfere with the production of the intrinsic factor needed for vitamin B12 absorption. As the cancer metastasizes to other structures, additional complications occur.
Assessment
In the early stages, the patient may complain of pain in his back or in the epigastric or retrosternal areas that’s relieved with nonprescription medications; however, he may not report this symptom because he doesn’t realize its significance. The patient typically reports a vague feeling of fullness, heaviness, and moderate abdominal distention after meals.
Depending on cancer progression, the patient may report weight loss due to appetite disturbance, nausea, and vomiting. He may report coffee-ground vomitus if the tumor is located in the cardia. He may also complain of weakness and fatigue. If the tumor is located in the proximal area of the stomach, he may experience dysphagia.
Palpation of the abdomen may disclose a mass or enlarged lymph nodes, especially the supraclavicular and axillary nodes.
Other assessment findings depend on the extent of the disease and the location of metastasis.
Other assessment findings depend on the extent of the disease and the location of metastasis.
Diagnostic tests
Barium swallow with fluoroscopy of the GI tract shows changes that suggest gastric cancer. Changes include a tumor or filling defect in the outline of the stomach, loss of flexibility and distensibility, and abnormal gastric mucosa with or without ulceration.
Gastroscopy with fiber-optic endoscope helps rule out other diffuse gastric mucosal abnormalities by allowing direct visualization. Gastroscopic biopsy permits evaluation of gastric mucosal lesions. Photography during gastroscopy provides a permanent record of gastric lesions that can later be used to judge disease progression and the effect of treatment.
Gastric acid stimulation test determines whether the stomach secretes acid properly.
Blood studies monitor the course of the disease, complications, and the effectiveness of treatment. These studies include a complete blood count (CBC), chemistry profiles, arterial blood gas analysis, liver function studies, and a carcinoembryonic antigen radioimmunoassay.
Certain other studies may rule out specific organ metastases. These include computed tomography scans, chest X-rays, liver and bone scans




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access