Foreign Body Obstruction and Management
Most cases of foreign-body airway obstruction in adults occur while they’re eating. In children, foreign-body airway obstruction occurs most often when they’re eating or playing and typically involves such items as balloons, small objects, or such foods as hot dogs, rounded candies, nuts, or grapes. In infants, airway obstruction typically results from a liquid.
Foreign bodies can cause mild or severe airway obstruction. If the obstruction is mild and the patient is coughing forcefully, there’s no reason to intervene; spontaneous coughing and breathing typically relieve the obstruction.1
If severe obstruction develops, you must intervene quickly to relieve the obstruction1 because anoxia resulting from the obstruction may cause brain damage and death within 4 to 6 minutes. Intervene by administering abdominal thrusts, also called the Heimlich maneuver, which uses a subdiaphragmatic abdominal thrust to create diaphragmatic pressure in the static lung below the foreign body sufficient to expel the obstruction. Abdominal thrusts are used in conscious adult patients who can’t speak, cough, or breathe.
If abdominal thrusts are ineffective, you may consider administering chest thrusts; this maneuver forces air out of the lungs, creating an artificial cough. Use chest thrusts for an obese patient, if you’re unable to encircle the patient’s abdomen, and for a patient who’s in the late stages of pregnancy.1 When administered to obese or pregnant patients who can’t speak, cough, or breathe, chest thrusts work by forcing air out of the lungs, creating an artificial cough.1
For infants, deliver repeated cycles of five back blows followed by five chest compressions until the foreign body is expelled or the infant becomes unresponsive. Abdominal thrusts aren’t recommended for infants because they may damage the infant’s liver.
If a patient is unconscious or becomes unconscious despite your efforts, start cardiopulmonary resuscitation (CPR) immediately.
Equipment
No special equipment is required.
Implementation
Determine whether the patient is choking by asking, “Are you choking?” If the victim indicates “yes” by nodding her head without speaking, she has a severe airway obstruction.1
Activate the emergency response system quickly if the patient is having difficulty breathing. If another person is present, have him activate the system.
Talk to the patient to keep her calm, and explain what you’re doing. Tell the patient that you’ll try to dislodge the foreign body.1
For A Conscious Adult or Child
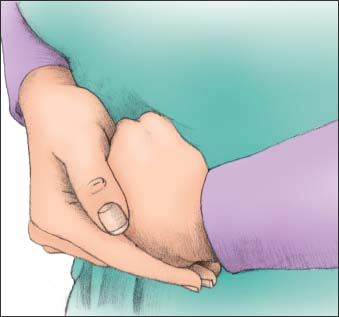
Standing behind the patient, wrap your arms around her waist. Make a fist with one hand, and place the thumb side against her abdomen, slightly above the umbilicus and well below the xiphoid process. Then grasp your fist with the other hand (as shown below).
Squeeze the patient’s abdomen using quick inward and upward thrusts. Each thrust should be a separate and distinct movement; each should be forceful enough to create an artificial cough that will dislodge an obstruction. Continue the abdominal thrust in rapid sequence until the obstruction is relieved or the patient becomes unresponsive.
Make sure you have a firm grasp on the patient because the patient may lose consciousness and need to be lowered to the floor.1 Support the head and neck to prevent injury. If the patient becomes unconscious, start CPR and follow the steps for an unconscious adult or child.
Examine the patient for injuries, such as ruptured or lacerated abdominal or thoracic viscera, resulting from the procedure.
For an Obese or Pregnant Adult
If the patient is conscious, stand behind her and place your arms under her armpits and around her chest.
Place the thumb side of your clenched fist against the middle of the sternum, avoiding the margins of the ribs and the xiphoid process (as shown at top of next column).

Grasp your fist with your other hand and perform a chest thrust with enough force to expel the foreign body. Continue until the patient expels the obstruction or loses consciousness. If the patient loses consciousness, carefully lower her to the floor and follow the steps outlined below for an unconscious adult or child.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
