Family Planning, Contraception, and Infertility
In this chapter, you’ll learn:
goals of family planning
various methods of contraception, including the advantages and disadvantages of each
surgical methods of family planning
issues related to elective termination of pregnancy
causes of infertility
treatments and procedures used to correct infertility.
A look at family planning
Family planning involves the decisions couples or individuals make regarding when (and if) they should have children, how many children to have, and how long to wait between pregnancies. Family planning also consists of choices to prevent or achieve pregnancy and to control the timing and number of pregnancies. Family planning is a personal topic that has many ethical, physical, emotional, religious, and legal implications. Effectiveness, cost, contraindications, and adverse effects for all contraceptives should be presented to the patient and her partner so that they can make an informed decision.
|
A look at contraception
Contraception is the deliberate prevention of conception, using a method or device to avert fertilization of an ovum.
Choosing a contraceptive
When discussing with a patient the contraceptive methods that are most appropriate for her and her partner, remember that a contraceptive should be safe, easily obtained, have minimal to no adverse effects, affordable, acceptable to the user and her partner, and free from effects on future pregnancies. In addition, couples should use a contraceptive that’s as close as possible to being 100% effective.
History lesson
Information from the patient’s menstrual and obstetric history should be used to determine which contraceptive method is best for her. The patient’s history is also used to plan appropriate patient teaching.
An assessment for family planning involves collecting a reproductive history, including:
|
interval between menses
duration and amount of flow
problems that occur during menses
number of previous pregnancies
number of previous births (and date of each)
duration of each pregnancy
type of each delivery
gender and weight of children when delivered
problems during previous pregnancies
problems after delivery.
Scope out potential complications
The patient’s health history may also identify potential risks of complications and help to determine whether hormonal contraceptives are safe for the patient to use. For example, a breast-feeding patient may be prescribed progesterone alone or a low-dose combination of hormonal contraceptives, which may cause her milk supply to decrease.
Factor in the partner
In some cases, the health of the patient’s sexual partner influences which contraception method is used. For example, if the
patient’s sexual partner is infected with HIV, ideally, she should practice abstinence. If this isn’t an option for your patient, encourage her to use a condom to prevent conception as well as infection transmission.
patient’s sexual partner is infected with HIV, ideally, she should practice abstinence. If this isn’t an option for your patient, encourage her to use a condom to prevent conception as well as infection transmission.
Implementing the chosen contraceptive
The effectiveness and safety of any contraceptive depends greatly on the patient’s knowledge of and compliance with the chosen method. The patient’s inability to understand proper use of the contraceptive device or an unwillingness to use it correctly or consistently may result in pregnancy. That’s why patient teaching is such an important component of family planning. (See Teaching tips on contraception.)
|
With proper instruction and information, the patient should be able to:
describe the use of the selected contraceptive correctly
describe adverse reactions to the selected contraceptive and state her responsibility to report any that occur
state that she’ll make an appointment for her next visit (if indicated)
express that the current method of birth control is an acceptable method for her.
 Education edge
Education edgeTeaching tips on contraception
Here are some points you should cover when teaching a patient about contraception:
Teach proper use of the selected contraceptive, and describe the procedure for the chosen method accurately.
Discuss possible adverse reactions. Direct the patient to report adverse reactions to her health care provider.
Stress the importance of keeping follow-up appointments. During follow-up visits, contraceptive use and adverse reactions are evaluated and it is possible a repeat Papanicolaou test may be performed. Follow-up visits also provide an opportunity to address any questions the patient may have.
Answer all questions in a manner that’s easily understood by the patient.
Methods of contraception
Contraceptive methods include abstinence, natural family planning methods, oral contraceptives, the morning-after pill (MAP) or emergency contraception, the intravaginal method, transdermal contraceptive patches, I.M. injections, intrauterine devices, intrauterine systems, and mechanical and chemical barrier methods.
Abstinence
Abstinence, or refraining from having sexual intercourse, has a 0% failure rate. It’s also the most effective way to prevent the transmission of sexually transmitted diseases (STDs). However, most individuals—especially adolescents—don’t consider it an option or a form of contraception. Abstinence should always be presented as an option to the patient in addition to information about other forms of contraception.
The plus side
Here are the advantages of abstinence:
It’s the only method that’s 100% effective against pregnancy and STDs.
It’s free.
There are no contraindications.
The minus side
Here are the disadvantages of abstinence:
Partners and peers may have negative reactions to it.
It requires commitment and self-control from both partners.
Natural family planning methods
Natural family planning methods are contraceptive methods that don’t use chemicals or foreign material or devices to prevent pregnancy. Religious beliefs may prevent some individuals from using hormonal or internal contraceptive devices. Others just prefer a more natural method of planning or preventing pregnancy. Natural family planning methods include the rhythm (calendar) method, basal body temperature method, cervical mucus (Billings) method, symptothermal method, ovulation awareness, and coitus interruptus.
|
Keeping count
For most natural family planning methods, the woman’s fertile days must be calculated so that she can abstain from
intercourse on those days. Various methods are used to determine the woman’s fertile period. The effectiveness of these methods depends on the patient’s and partner’s willingness to refrain from sex on the female partner’s fertile days. Failure rates vary from 10% to 20%.
intercourse on those days. Various methods are used to determine the woman’s fertile period. The effectiveness of these methods depends on the patient’s and partner’s willingness to refrain from sex on the female partner’s fertile days. Failure rates vary from 10% to 20%.
Rhythm method
The rhythm, or calendar, method requires that the couple refrain from intercourse on the days that the woman is most likely to conceive based on her menstrual cycle. This fertile period usually lasts from 3 or 4 days before until 3 or 4 days after ovulation.
Dear diary
Teach the woman to keep a diary of her menstrual cycle to determine when ovulation is most likely to occur. She should do this for 6 consecutive cycles. To calculate her safe periods, tell her to subtract 18 from the shortest cycle and 11 from the longest cycle that she has documented. For instance, if she had 6 menstrual cycles that lasted 26 to 30 days, her fertile period would be from the 8th day (26 minus 18) to the 19th day (30 minus 11). To ensure that pregnancy doesn’t occur, she and her partner should abstain from intercourse during days 8 to 19 of her menstrual cycle. During those fertile days, she and her partner may also choose to use contraceptive foam. (See Using the calendar method.)
|
The plus side
Here are the advantages of the rhythm method:
No drugs or devices are needed.
It’s free.
It may be acceptable to members of religious groups that oppose birth control.
It encourages couples to learn more about how the female body functions.
It encourages communication between partners.
It can also be used to plan a pregnancy.
The minus side
Here are the disadvantages of the rhythm method:
It requires meticulous record-keeping as well as an ability and willingness for the woman to monitor her body changes.
It restricts sexual spontaneity during the woman’s fertile period.
It requires extended periods of abstinence from intercourse.
It’s only reliable for women with regular menstrual cycles.
It may be unreliable during periods of illness, infection, or stress.
Ovulation can resume as early as 4 weeks after the birth of a baby; the rhythm (calendar) method would be unreliable during the postpartum period or if a woman is breast-feeding until normal cycles resume.
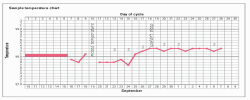
Using the calendar method
This illustration demonstrates how the calendar method would be used to determine the woman’s fertile period (ovulation) and when she should abstain from coitus.
|
Basal body temperature
Just before the day of ovulation, a woman’s basal body temperature (BBT) falls about one-half of a degree. At the time of ovulation, her BBT rises a full degree because of progesterone influence.
Ups and downs, highs and lows
To use the BBT method of contraception, a woman must take her temperature every morning before sitting up, getting out of bed, or beginning her morning activity. (See Teaching a patient how to take BBT, pages 68 and 69.) By recording this daily temperature, she can see a slight dip and then an increase in body temperature. The increase in temperature indicates that she has
ovulated. She should refrain from intercourse for the next 3 days. Three days is significant because this is the lifespan of a discharged ovum. Because sperm can survive in the female reproductive tract for 4 days, the BBT method of contraception is typically combined with the calendar method so that the couple can abstain from intercourse a few days before ovulation as well.
ovulated. She should refrain from intercourse for the next 3 days. Three days is significant because this is the lifespan of a discharged ovum. Because sperm can survive in the female reproductive tract for 4 days, the BBT method of contraception is typically combined with the calendar method so that the couple can abstain from intercourse a few days before ovulation as well.
Various variables
One problem with this method is that many things can affect BBT. The woman may forget and take her temperature after rising out of bed or she may have a slight illness. These situations cause a rise in temperature. If the woman changes her daily routine, the change in activity could also affect her body temperature, which may lead her to mistakenly interpret a fertile day as a safe day and vice versa.
|
The plus side
Here are the advantages of the BBT method:
It’s inexpensive. The only expense involved is the cost of a BBT thermometer, which is calibrated in tenths of a degree.
No drugs are needed.
It may be acceptable to members of religious groups that oppose birth control.
It encourages couples to learn more about how the female body functions.
It encourages communication between partners.
It can also be used to plan a pregnancy.
The minus side
Here are the disadvantages of the BBT method:
It requires meticulous record-keeping and an ability and willingness to monitor the woman’s body changes.
It restricts sexual spontaneity during the woman’s fertile period.
It requires extended periods of abstinence from intercourse.
It’s reliable only for women with regular menstrual cycles.
It may be unreliable during periods of illness, infection, or stress.
It’s contraindicated in women who have irregular menses.
It is unreliable following the birth of a baby until regular menstrual cycles have resumed.
Cervical mucus method
The cervical mucus method (also known as the Billings method) predicts changes in the cervical mucus during ovulation.
During nonfertile times of a woman’s menstrual cycle, cervical mucus is thick, sticky, opaque, and impervious (inhospitable) to sperm. Just prior to ovulation, cervical mucus becomes thin, colorless, copious in amount, and will stretch between two fingers approximately 8 to 10 cm (3 to 4 in.). This thin, stretchable mucus (also known as spinnbarkeit) is favorable to sperm and facilitates transport of sperm through the cervix into the uterus.
Slippery peaks
During the peak of ovulation, the cervical mucus becomes slippery and stretches at least 2.5 cm (1 in.) before the strand breaks. Breast tenderness and anterior tilt of the cervix also occur with ovulation. The fertile period consists of all the days that the cervical mucus is copious and the 3 days after the peak date. During these days, the woman and her partner should abstain from intercourse to avoid conception.
Consistently checking consistency
Cervical mucus must be assessed every day for changes in consistency and amounts to be sure that those changes signify ovulation. Assessing cervical mucus after intercourse is unreliable because seminal fluid has a watery, postovulatory consistency, which can be confused with ovulatory mucus.
The plus side
Here are the advantages of the cervical mucus method:
No drugs or devices are needed.
It’s free.
It may be acceptable to members of religious groups that oppose birth control.
It encourages couples to learn more about how the female body functions.
It encourages communication between partners.
It can also be used to plan a pregnancy.
There are no contraindications.
The minus side
Here are the disadvantages of the cervical mucus method:
It requires meticulous record-keeping and an ability and willingness to monitor the woman’s body changes.
It restricts sexual spontaneity during the woman’s fertile period.
It requires extended periods of abstinence from intercourse.
It’s reliable only for women with regular menstrual cycles.
It may be unreliable during periods of illness, infection, or stress.
It is unreliable during the postpartum period until regular menstrual cycles have resumed or while breast-feeding.
 Education edge
Education edgeTeaching a patient how to take BBT
Here are tips to help you teach your patient about recording BBT. Remind the patient that BBT is lower during the first 2 weeks of the menstrual cycle, before ovulation. Immediately after ovulation, the temperature begins to rise. It continues to rise until it’s time for the next menses. This rise in temperature indicates that progesterone has been released into the system, which, in turn, means that the woman has ovulated.
Charting BBT doesn’t predict the exact day of ovulation; it just indicates that ovulation has occurred. However, this can be used to help the patient to monitor her ovulatory pattern and give her a timeframe during which ovulation occurs.
Getting started
Tell your patient to follow these instructions for taking BBT:
Advise the patient to chart the days of menstrual flow by darkening the squares above the 98° F (36.7° C) mark. She should start with the first day of her menses (day 1) and then take her temperature each day after her menses ends.
Tell the patient to use a thermometer that measures tenths of a degree.
Instruct the patient to take her temperature as soon as she wakes up. Tell her that it’s important to do this at the same time each morning.
The patient should then place a dot on the graph’s line that matches the temperature reading. (Tell her not to be surprised if her waking temperature before ovulation is 96° or 97° F [35.6° or 36.1° C].) If she forgets to take her temperature on 1 day, instruct her to leave that day blank on the graph and not to connect the dots.
Instruct her to make notes on the graph if she misses taking her temperature, feels sick, can’t sleep, or wakes up at a different time. Advise her also that if she’s taking any medicine—even aspirin—it may affect her temperature. Remind her to mark the dates when she has sexual intercourse.
Sample chart
Look over the sample temperature chart, recorded by “Susan Jones.” Ms. Jones used an S to record sexual intercourse and made notes showing she had insomnia on September 27. She forgot to take her temperature on September 19. Notice that she didn’t connect the dots on this day. Her temperature dipped on September 24 (day 15 of the cycle) and began rising afterward.
Of course, your patient’s chart will be larger and will probably include temperatures over 99.3° F (37.4° C) and under 97° F.
Symptothermal method
The symptothermal method combines the BBT method with the cervical mucus method. The woman takes her daily temperature and watches for the rise in temperature that signals the onset of ovulation. She also assesses her cervical mucus every day. The couple abstains from intercourse until 3 days after the rise in basal temperature or the fourth day after the peak day (indicating ovulation) of cervical mucus because these signs signify the
woman’s fertile period. Combining these two methods is more effective than using either method alone.
woman’s fertile period. Combining these two methods is more effective than using either method alone.
|
The plus side
Here are the advantages of the symptothermal method:
It’s inexpensive. The only expense involved is the cost of a BBT thermometer, which is calibrated in tenths of a degree.
No drugs are needed.
It may be acceptable to members of religious groups that oppose birth control.
It encourages patients and their partners to learn more about how the female body functions.
It encourages communication between partners.
It can also be used to plan a pregnancy.
The minus side
Here are the disadvantages of the symptothermal method:
It requires meticulous record-keeping and ability and willingness of a woman to monitor body changes.
It restricts sexual spontaneity during the woman’s fertile period.
It requires extended periods of abstinence from intercourse.
It’s reliable only for women with regular menstrual cycles.
It may be unreliable during periods of illness, infection, or stress.
It is unreliable during the postpartum period until regular menstrual cycles have resumed, or while breast-feeding.
Ovulation awareness
Over-the-counter ovulation detection kits determine when ovulation occurs by measuring luteinizing hormone (LH) in the urine. Usually, during each menstrual cycle, LH levels rise suddenly (called an LH surge), causing an ovum to be released from the ovary 24 to 36 hours later (ovulation). This test determines the midcycle surge of LH, which can be detected in the urine as early as 12 to 24 hours after ovulation. These kits are about 98% to 100% accurate, but they’re fairly expensive to use as a primary means of birth control. (See Performing a home ovulation test.)
|
The plus side
Here are the advantages of the ovulation awareness method:
It’s an easier way to determine ovulation than the BBT or cervical mucus methods.
It may be less offensive to a woman than the cervical mucus method.
It has a high rate of accuracy.
There are no contraindications.
|
The minus side
Here are the disadvantages of the ovulation awareness method:
It’s expensive.
It requires extended periods of abstinence from intercourse.
It’s reliable only for women with regular menstrual cycles.
Coitus interruptus
Coitus interruptus, one of the oldest known methods of contraception, involves withdrawal of the penis from the vagina during intercourse before ejaculation. However, because pre-ejaculation fluid that’s deposited outside the vagina may contain spermatozoa, fertilization can occur.
 Education edge
Education edgePerforming a home ovulation test
A home ovulation test helps the patient determine the best time to try to become pregnant or to prevent pregnancy by monitoring the amount of LH that’s found in her urine. These test kits can be purchased over-the-counter.
Normally, during each menstrual cycle, levels of LH rise suddenly, causing an egg to be released from the ovary 24 to 36 hours later.
Getting ready
Tell your patient to follow these instructions before performing a home ovulation test:
Read the kit’s directions thoroughly before performing the test.
Before testing, calculate the length of the menstrual cycle. Count from the beginning of one menses to the beginning of the next menses. (The patient should count her first day of bleeding as day 1. She can use a chart such as the one shown at right to determine when to begin testing.)
This test can be performed any time of the day or night, but it should be performed at the same time every day.
Don’t urinate for at least 4 hours before taking the test, and don’t drink a lot of fluids for several hours before the test.
Taking the test
Tell your patient to follow these instructions for performing a home ovulation test:
Remove the test stick from the packet.
Sit on the toilet and direct the absorbent tip of the test stick downward and directly into the urine stream for at least 5 seconds or until it’s thoroughly wet.
Be careful not to urinate on the window of the stick.
Alternatively, urinate in a clean, dry cup or container and then dip the test stick (absorbent tip only) into the urine for at least 5 seconds.
Place the stick on a clean, flat, dry surface.
Reading the results
Explain to your patient the following instructions for reading home ovulation test results:
Wait at least 5 minutes before reading the results. When the test is finished, a line appears in the small window (control window).
If there’s no line in the large rectangular window (test window) or if the line is lighter than the line in the small rectangular window (control window), the patient hasn’t begun an LH surge. She should continue testing daily.
If she sees one line in the large rectangular window that’s similar to or darker than the line in the small window, she’s experiencing an LH surge.
This means that ovulation should occur within the next 24 to 36 hours.
Once the patient has determined that she’s about to ovulate, she’ll know she’s at the start of the most fertile time of her cycle and should use this information to plan accordingly.
|
The plus side
Here are the advantages of the coitus interruptus method:
It’s free.
It doesn’t involve record-keeping.
There are no contraindications.
The minus side
Here are the disadvantages of the coitus interruptus method:
It isn’t reliable.
It restricts sexual spontaneity.
Certain patient populations may not be appropriate for natural family planning methods. These may include adolescents, women who are not in monogamous relationships, women with irregular menses, and women whose partners are not interested in active participation in natural family planning.
Combined oral contraceptives
Combined oral contraceptives (birth control pills) are hormonal contraceptives that consist of synthetic estrogen and progesterone. The estrogen suppresses production of follicle-stimulating hormone (FSH) and LH, which, in turn, suppresses ovulation. The progesterone complements the estrogen’s action by causing a decrease in cervical mucus permeability, which limits sperm’s access to the ova. Progesterone also decreases the possibility of implantation by interfering with endometrial proliferation.
Dosage duo
There are two types of combined oral contraceptives:
 Monophasic oral contraceptives provide fixed doses of estrogen and progesterone throughout a 21-day cycle. These preparations provide a steady dose of estrogen but an increased amount of progestin during the last 11 days of the menstrual cycle.
Monophasic oral contraceptives provide fixed doses of estrogen and progesterone throughout a 21-day cycle. These preparations provide a steady dose of estrogen but an increased amount of progestin during the last 11 days of the menstrual cycle. Triphasic oral contraceptives maintain a cycle more like a woman’s natural menstrual cycle because they vary the amount of estrogen and progestin throughout the cycle. Triphasic oral contraceptives have a lower incidence of breakthrough bleeding than monophasic oral contraceptives.
Triphasic oral contraceptives maintain a cycle more like a woman’s natural menstrual cycle because they vary the amount of estrogen and progestin throughout the cycle. Triphasic oral contraceptives have a lower incidence of breakthrough bleeding than monophasic oral contraceptives.
|
Small but powerful
A mini pill is a progestin-only oral contraceptive (Micronor and Ovrette) available for women who can’t take estrogen-based
pills because of a history of thrombophlebitis. This type of pill is taken every day—even when the woman has her menses. Progestins in the pill inhibit the development of the endometrium, thus preventing implantation. Progestin-only pills may also be used by women who are breast-feeding.
pills because of a history of thrombophlebitis. This type of pill is taken every day—even when the woman has her menses. Progestins in the pill inhibit the development of the endometrium, thus preventing implantation. Progestin-only pills may also be used by women who are breast-feeding.
The mini pill must be taken at exactly the same time each day. If a dose is missed, another form of contraception, such as a barrier or chemical method, should be used for the remainder of the menstrual cycle.
21- or 28-day package deals
Monophasic and triphasic oral contraceptives are dispensed in either 21- or 28-day packs. The first pill is usually taken on the first Sunday following the start of a woman’s menses, but it’s possible to start oral contraceptives on any day. For a woman who has recently given birth, oral contraceptives can be started on the first Sunday 2 weeks after delivery. Patients should be advised to use an additional form of contraception for the first week after starting an oral contraceptive because the drug doesn’t take full effect for 7 days. (See Teaching tips on oral contraceptives.)
Birth control pills that are prescribed in a 21-day dispenser allow the woman to take a pill every day for 3 weeks. She should expect to start her menstrual flow about 4 days after she takes a cycle of pills. The 28-day pills are packaged with 21 days of birth control pills and 7 days of placebos. The woman starts the new pack of pills when she finishes the last pack, eliminating the risk of forgetting to start a new pack.
 Education edge
Education edgeTeaching tips on oral contraceptives
Be sure to include these tips when teaching patients about oral contraceptives:
Inform the patient about possible adverse reactions, such as fluid retention, weight gain, breast tenderness, headache, breakthrough bleeding, chloasma, acne, yeast infection, nausea, and fatigue. It may be necessary to change the type or dosage of the contraceptive to relieve these adverse reactions.
Instruct the patient on the dietary needs of a woman who’s taking an oral contraceptive. Tell her to increase her intake of foods high in vitamin B6 (wheat, corn, liver, meat) and folic acid (liver; green, leafy vegetables). About 20% to 30% of oral contraceptive users have dietary deficiencies of vitamin B6 and folic acid. Moreover, health care professionals speculate that oral contraceptive users should also increase their intake of vitamins A, B2, B12, C, and niacin.
Advise the patient to use an additional form of contraception for the first 7 days after starting the drug because it doesn’t take full effect for 7 days.
Advise the patient to use an additional form of contraception when taking antibiotics until the beginning of a normal menstrual period.
It’s seasonal
A newer oral contraceptive on the market is a combination of levonorgestrel and ethinyl estradiol in which one tablet is taken daily for 12 weeks (brand name Seasonale). This pill extends the time between periods, allowing a woman to have a period four times a year as opposed to monthly.
The plus side
Here are the advantages of oral contraceptives:
Monophasic and triphasic oral contraceptives are 99.5% effective with “perfect use.” The failure rate is about 3%; failure usually occurs because the woman forgets to take the pill or because of other individual differences in the woman’s physiology.
They don’t inhibit sexual spontaneity.
They may reduce the risk of endometrial and ovarian cancer, ectopic pregnancy, ovarian cysts, and noncancerous breast tumors.
They decrease the risk of pelvic inflammatory disease (PID) and dysmenorrhea.
They regulate the menstrual cycle and may diminish or eliminate premenstrual tension.
The minus side
Here are the disadvantages of oral contraceptives:
They don’t protect the woman or her partner from STDs.
They must be taken daily.
They can be expensive with a copay required every month.
Illnesses that cause vomiting may reduce their effectiveness.
Most combination oral contraceptives are contraindicated in women who are breast-feeding as they may reduce milk supply.
Patients with a family history of stroke, coronary artery disease, thrombohemolytic disease, or liver disease should have additional testing prior to being prescribed estrogen-containing oral contraceptives. Oral contraceptives are contraindicated in patients who have a personal history of thromboembolic event such as deep vein thrombosis or pulmonary embolism.
Women who are older than age 40, and those who have a history of or have been diagnosed with diabetes mellitus, elevated triglyceride or cholesterol level, breast or reproductive tract malignancy, high blood pressure, obesity, seizure disorder, sickle cell disease, mental depression, and migraines or other vascular-type headaches, should
be strongly cautioned about taking oral contraceptives for birth control. The possible side effects of oral contraceptives may be more severe in women who fall under these categories.
A patient older than age 35 is at increased risk for a fatal heart attack if she smokes more than 15 cigarettes per day and takes oral contraceptives.
Adverse effects include nausea, headache, weight gain, depression, mild hypertension, breast tenderness, breakthrough bleeding, and monilial (yeast) vaginal infections.
When a woman wants to conceive, she may not be able to for up to 8 months after stopping oral contraceptives. The pituitary gland requires a recovery period to begin the stimulation of cyclic gonadotropins, such as FSH and LH, which help regulate ovulation. In addition, many practitioners recommend that women not become pregnant within 2 months of stopping oral contraceptives.
Morning-after pill
Also called emergency contraception, the MAP prevents pregnancy in the event of unprotected sexual intercourse or failure of a birth control method (such as a broken condom). It may be obtained from various doctors’ offices and family planning clinics. The MAP is a pregnancy prevention measure, not an abortion pill.
The MAP is given as two doses of hormones: progesterone alone, estrogen alone, or a combination of both. The first dose must be taken within 72 hours of sexual intercourse; a second dose is taken 12 hours later. A woman may be prescribed a certain number of oral hormonal contraceptive pills from a birth control pack (estrogen and progesterone combination) or she may be prescribed a “plan B” pack, which contains 0.75 mg of levonorgestrel.
Medications for nausea may also be prescribed, and the woman is instructed to return to the office or clinic in 3 weeks. She must also be instructed to use a birth control method consistently until her menstrual period begins.
The plus side
Here are the advantages of the MAP:
It’s 75% to 95% effective, depending on which product is used, when in the cycle intercourse occurred, how soon the woman uses the method, and whether she has had unprotected intercourse within the past 72 hours.
It doesn’t inhibit sexual spontaneity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access