F
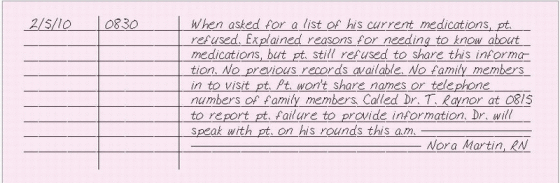
FAILURE TO PROVIDE INFORMATION
You may occasionally encounter a patient who refuses to provide accurate or complete information about his health history, current medications, or treatments. He may be uncooperative for various reasons: He thinks too many caregivers have asked him the same questions too many times, he doesn’t understand the significance of the information, he’s fearful or disoriented, or he’s suspicious of why you want him to divulge personal information. Alternatively, he may have severe pain, a psychiatric problem, or a language barrier. In such situations, try to obtain the information from other sources or forms.
ESSENTIAL DOCUMENTATION
Clearly document any trouble you’ve had communicating with the patient. Record his responses using his own words. Include your interventions or explanations of the importance of this information in order to provide the patient with the best possible care. Document the name of the doctor you notified about the patient’s refusal to share information and the time of notification. Write down other sources of information, such as family members or previous records.
|
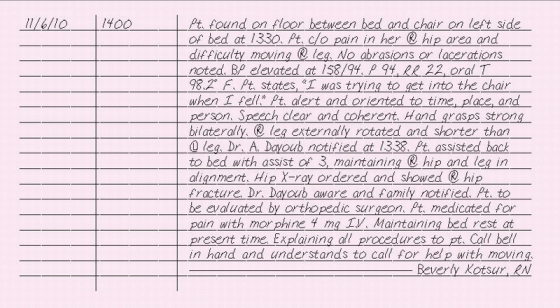
FALLS, PATIENT
Falls are a major cause of injury and death among older patients. In fact, the older the person, the more likely he’ll die due to a fall or its complications. In acute care hospitals, 85% of all inpatient incident reports are related to falls; of those who fall, 10% fall more than once and 10% experience a fatal fall. In nursing homes, approximately 60% of residents fall every year and about 40% of those residents experience more than one fall.
If your patient falls despite preventative measures, stay with him and don’t move him until you’ve performed a head-to-toe assessment and checked his vital signs. Assign another person to notify the doctor. Provide any emergency measures necessary, such as securing an airway, controlling bleeding, or stabilizing a deformed limb. Ask the patient or a witness what happened. Ask the patient if he’s in pain or hit his head. If you don’t detect any problems, return the patient to bed with the help of another person.
ESSENTIAL DOCUMENTATION
If a patient falls despite precautions, be sure to file an incident report and chart the event. (See “Incident report,” pages 205 to 207.) Record how the patient was found and the time he was discovered. Document an objective assessment, avoiding any judgments or opinions. Assess the patient and record any bruises, lacerations, or abrasions. Describe any pain or deformity in the extremities, particularly the hip, arm, leg, or lumbar spine. Record vital signs, including orthostatic blood pressure. Document your patient’s neurologic assessment. Include slurred speech, weakness in the extremities, or a change in mental status. Record the name of the doctor
and other persons notified, such as family members, and the time of noti-fication. Include instructions or orders given. Also document any patient education.
and other persons notified, such as family members, and the time of noti-fication. Include instructions or orders given. Also document any patient education.
|
FALLS, PRECAUTIONS
Patient falls resulting from slips, slides, knees giving way, fainting, or tripping over equipment can lead to prolonged hospitalization, increased hospital costs, and liability problems. Because falls cause so many problems, your facility may require you to assess each patient for his risk of falling and to take measures to prevent falls. (See Reducing the risk of falls, page 149.) If your facility requires a risk assessment form for patients, complete it and keep it in the patient’s chart. (See Risk assessment for falls, page 150.) Those at risk require a care plan reflecting interventions to prevent falls. (See Reducing your liability in patient falls, page 151.)
ESSENTIAL DOCUMENTATION
Record the time and date of your entry. Describe the reasons for implementing fall precautions for your patient, such as a high score on a risk for falls assessment tool. Document your interventions, such as frequent toileting, reorienting the patient to his environment, and placing needed objects within his reach. Include the patient’s response to these interventions. Note measures taken to alert other health care workers of the risk
for falls, such as placing a band on the patient’s wrist and communicating this risk on the patient’s Kardex. Record any patient and family teaching and their level of understanding. In some facilities, patient and family education may be documented on an education flow sheet.
for falls, such as placing a band on the patient’s wrist and communicating this risk on the patient’s Kardex. Record any patient and family teaching and their level of understanding. In some facilities, patient and family education may be documented on an education flow sheet.
REDUCING THE RISK OF FALLS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access