Electrocardiogram, Signal-Averaged
Signal-averaged electrocardiography (ECG) helps to identify patients at risk for sustained ventricular tachycardia. Because this cardiac arrhythmia can be a precursor of sudden death after a myocardial infarction (MI), the results of signal-averaged ECG can allow appropriate preventive measures.1
Using a computer-based ECG, signal averaging detects low-amplitude signals or late electrical potentials, which reflect slow conduction or disorganized ventricular activity through abnormal or infarcted regions of the ventricles. The signal-averaged ECG is developed by recording the noise-free surface ECG in three specialized leads for several hundred beats. (See Placing electrodes for signal-averaged ECG.) Signal averaging enhances signals that would otherwise be missed because of increased amplitude and sensitivity to ventricular activity. For instance, on the standard 12-lead ECG, “noise” created by muscle tissue, electronic artifacts, and electrodes masks late potentials, which have a low amplitude. This procedure identifies the risk for sustained ventricular tachycardia in patients with malignant ventricular tachycardia, a history of MI, unexplained syncope, nonischemic congestive cardiomyopathy, or nonsustained ventricular tachycardia.
Equipment
Signal-averaged ECG machine ▪ signal-averaged computer ▪ record of patient’s surface ECG for 200 to 300 QRS complexes ▪ three bipolar electrodes or leads ▪ Optional: moist cloth, soap, clippers, gloves.
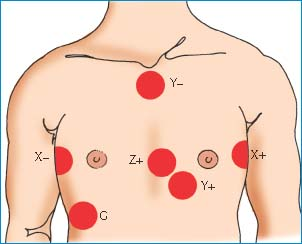
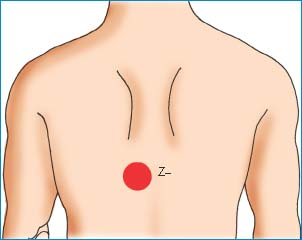
Placing Electrodes for Signal-Averaged ECG
To prepare your patient for a signal-averaged electrocardiogram (ECG), place the electrodes in the X, Y, and Z orthogonal positions, as shown here. These positions bisect one another to provide a three-dimensional, composite view of ventricular activation.
Implementation
Verify the doctor’s order.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access