Documenting care
Proper nursing documentation provides a record of your nursing care. Detailed standards have been developed by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) to guide the documentation of a patient’s care up to and after death. These standards emphasize the integration of services from a variety of providers. They include assessment and care of patients, leadership, management of human resources, and ongoing data collection.
Clearly, documentation is as important for a dying patient as it is for any other patient. In the area of end-of-life care, certain issues in documentation deserve special mention. These include understanding the type of documentation you’ll be using and documenting pain control, advance directives, Medicare requirements, organ donation, and documentation after death.
Documenting pain control
Documentation of pain control is essential as the patient progresses through the dying process. When charting pain levels and characteristics of discomfort, document the location of the pain and whether it’s internal, external, localized, or diffuse. Using the patient’s own words, describe his pain, emphasizing how long the pain lasts, how often it occurs, as well as his ranking of the pain using a numerical, visual, or verbal scale.
Also describe the patient’s behaviors associated with the pain, and record changes in blood pressure, dilated pupils, shortness of breath, elevated heart rate, and diaphoresis. Chart positions and measures that relieve or worsen
the pain. A pain flowsheet can be invaluable in documenting pain occurrence and describing its characteristics. It can be particularly beneficial for families involved in caring for a loved one at home because they may be overwhelmed by a lengthy, detailed questionnaire. A pain flowsheet should include at least the following five categories:
the pain. A pain flowsheet can be invaluable in documenting pain occurrence and describing its characteristics. It can be particularly beneficial for families involved in caring for a loved one at home because they may be overwhelmed by a lengthy, detailed questionnaire. A pain flowsheet should include at least the following five categories:
Patient-controlled analgesia: Flowsheet documentation
Although each facility will vary slightly in its requirements, certain elements are typically included in documenting patient-controlled analgesia (PCA) on a flowsheet:
Type of drug used, including mixture amounts
Time of cartridge insertion
PCA settings, including lockout interval
Dose volume
Continuous settings
4-hour limit
Vital signs
Rating of level of sedation
Rating of level of pain
Additional doses given
Total milliliters of analgesic given
Total milliliters remaining in medication cartridge
date and time of every occurrence of pain
patient rating of pain from 0 to 10 when pain occurs
patient behaviors with each occurrence of pain
patient rating of pain from 0 to 10 after intervention to relieve pain
description of drugs given or other measures taken for pain relief.
As the patient continues to move through the dying process, he may use patient-controlled analgesia. This lets the patient self-administer boluses of an opioid analgesic intravenously, subcutaneously, or epidurally within prescribed limits. Patient-controlled analgesia increases the patient’s sense of control, reduces his anxiety, reduces the amount of analgesic used, and increases pain control. This type of pain relief is particularly effective when used with terminal cancer patients.
When documenting the use of patient-controlled analgesia with a dying patient, make sure to include the name of the opioid used, the lockout interval, the maintenance dose used, the amount of drug the patient receives when he activates the device, and the amount of opioid used during your shift. Record the patient’s assessment of pain relief, patient teaching performed, vital signs, and level of consciousness, as well as observations of the insertion site. (See Patient-controlled analgesia: Flowsheet documentation.)
Advance directives
An advance directive is a legal document executed by the patient while he is of sound mind that dictates his wishes should he become incapacitated and unable to make decisions. Under ideal circumstances, the patient has discussed his wishes with his family members and they agree to his desired outcomes. However, there may be situations in which family members contest the patient’s wishes for the advance directive. The legality of the situation dictates that the living will be upheld. The family’s rights will be superseded by the living will.
Should such contention occur, notify the physician, the nursing supervisor, and the facility’s risk manager. Document conversations held with the family members, quoting their exact words. Record an assessment of the family dynamics. Document the name and department of all personnel notified. Consider making a referral to the facility’s ethics committee or patient advocate, and document all referrals made.
If the patient wishes not to be resuscitated, inform the practitioner and request that a signed do-not-resuscitate (DNR) order be placed in his chart.
Even if a patient has an advance directive, it should be reviewed yearly and updated as needed. The advance directive will only become effective if the conditions under which the patient has defined the document to be activated have occurred. The advance directive may be revoked by the patient at any time. If the patient decides to revoke his advance directive, place a copy of his written revocation in the medical record, or sign and date a statement in the patient’s own words explaining that the patient made the request orally. Include names of witnesses who heard the patient revoke his advance directive. Record that the physician, risk manager, and nursing supervisor were notified of the revocation.
Interdisciplinary team
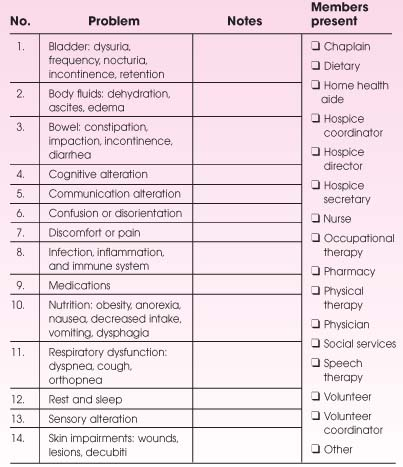
The emphasis of hospice and palliative care is on the benefits of all disciplines working together to assist the patient and family to achieve their goals. Documentation of interactions of interdisciplinary team members is essential. In hospitals, the progress note is typically used by all disciplines and can serve this function. In extended care facilities, home care, and inpatient hospice settings, it may be helpful to have a form dedicated to this function. The form should identify which problem was discussed, based on the care plan established for that patient. The specific people involved should also be identified; include the patient or family when appropriate.
The note should include the interventions agreed upon, which team members will carry them out, and an expected timeline for re-evaluation. (See Interdisciplinary team meeting record.)
The note should include the interventions agreed upon, which team members will carry them out, and an expected timeline for re-evaluation. (See Interdisciplinary team meeting record.)
Medicare measures
Documentation is an integral part of the process of providing hospice care to a patient under the Medicare hospice benefit. Hospice care specifically
refers to services provided for a terminally ill patient who has been judged by two physicians as having a life expectancy of 6 months or less.
refers to services provided for a terminally ill patient who has been judged by two physicians as having a life expectancy of 6 months or less.
To access Medicare’s hospice benefits, when hospice care is desired, the patient must file an election statement with a Medicare-certified hospice. When hospice care is elected by the patient, he waives all rights to Medicare payments for treatments related to the terminal illness and instead receives hospice care for the terminal illness. However, if the patient also needs care for conditions unrelated to his terminal illness, he can receive hospice as well as Medicare-reimbursed health benefits.
Hospice in nursing homes
Hospice care is also being used to provide skills and services in nursing homes. The National Hospice Organization has published guidelines to help determine the appropriateness of a chronically ill patient to receive hospice care. Documentation is particularly important in this instance because the guidelines require frequent reevaluation of the patient’s condition to monitor disease progression. Based on the guidelines, an eligible patient would be unable to bathe properly, have urinary and fecal incontinence, be unable to ambulate without assistance, be unable to dress without assistance, and be unable to speak or communicate meaningfully.
Once a nursing home resident is identified as having a limited life expectancy, it’s important to recognize that the Medicare hospice benefit can assist in providing palliative management of the dying patient’s symptoms, paying particular attention to the patient’s increased daily needs and supplying bereavement services. (See Services covered by the Medicare hospice benefit.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree