Diverticulitis
By age 80, more than 50% of the U.S. population has acquired the condition called diverticulosis in which individual outpouchings, or diverticula, present in the mucosa and submucosa of the muscular wall of the large intestine herniate through weak sites. Most cases are asymptomatic and are discovered incidental to colonoscopy or barium enema. It is believed to be caused by a diet low in fiber, resulting in chronic constipation. Because of dietary factors, it is a condition seldom found in developing countries, where a more fibrous diet is the norm. Poor bowel habits, such as ignoring the urge to defecate, contribute to the development of diverticular disease. Approximately 20% of all people with diverticulosis develop symptomatic disease.
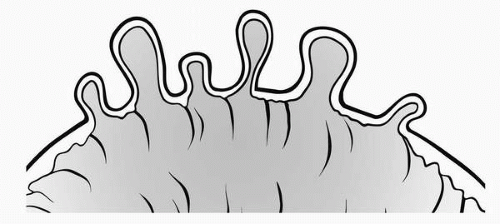
The three types of diverticular disease are true, false, and pseudodiverticula. Most diverticula occur in the distal sigmoid colon in the presence of long-standing constipation. From the prolonged effort of moving small, hard stools along, the muscular layer becomes hypertrophied, rigid, thick, and fibrous. High intraluminal pressure is needed to propel stool through the colon, but this same pressure can force the mucosa through a preexisting area of weakness in the wall, producing a diverticula. Most individuals are asymptomatic and require no treatment except for a high fiber diet or fiber supplements such as bran. Some may complain of abdominal pain lasting hours to days and relieved by passing flatus or feces. Because these events are often accompanied by either diarrhea or constipation, a constellation of symptoms also found with the condition of irritable bowel, it is speculated that there may be a relationship between the two diseases.
 High intraluminal pressure is needed to propel stool through the colon, but this same pressure can force the mucosa through a preexisting area of weakness in the wall, producing a diverticula.
High intraluminal pressure is needed to propel stool through the colon, but this same pressure can force the mucosa through a preexisting area of weakness in the wall, producing a diverticula.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access