Diabetes mellitus
A chronic disease of absolute or relative insulin deficiency or resistance, diabetes mellitus is characterized by disturbances in carbohydrate, protein, and fat metabolism. Insulin transports glucose into the cells for use as energy and storage as glycogen. It also stimulates protein synthesis
and free fatty acid storage in the adipose tissues. Insulin deficiency compromises the body tissues’ access to essential nutrients for fuel and storage.
and free fatty acid storage in the adipose tissues. Insulin deficiency compromises the body tissues’ access to essential nutrients for fuel and storage.
The disorder occurs in two primary forms: type 1, characterized by absolute insufficiency, and the more prevalent type 2, characterized by insulin resistance with varying degrees of insulin secretory defects.
Onset of type 1 usually occurs before age 30, although it may occur at any age; the patient is usually thin and requires exogenous insulin and dietary management to control blood glucose levels. Type 2 usually occurs in obese adults older than age 40, although it’s commonly seen in North American youths. Type 2 diabetes mellitus is often treated with diet and exercise in combination with antidiabetic drugs; treatment may include insulin therapy.
Diabetes mellitus is thought to affect about 8% of the U.S. population (16 million diagnosed cases). About half of those affected are undiagnosed. Incidence is higher in males than females and increases with age.
Causes
The causes of type 1 and type 2 diabetes mellitus remain unknown. Genetic factors may influence the development of both types. Autoimmune disease and viral infections may be risk factors in type 1 diabetes mellitus.
Risk factors for type 2 diabetes include:
obesity (BMI greater than or equal to 27 kg/m2)
family history of diabetes
history of gestational diabetes, previous glucose intolerance, or delivery of a baby weighing more than 9 lb (4.1 kg)
high-density lipoprotein levels less than or equal to 35 mg/dl or triglycerides greater than or equal to 250 mg/dl
hypertension (blood pressure is greater than or equal to 140/90 mm Hg in adults)
age (greater than or equal to 45).
Complications
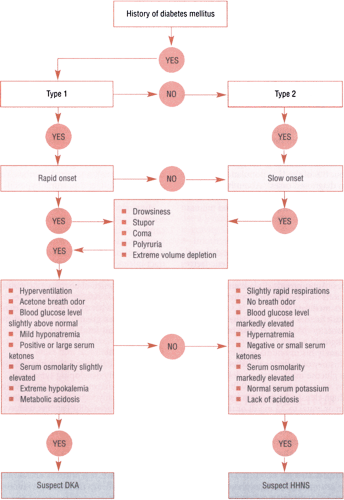
Two acute metabolic complications of diabetes are diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic nonketotic syndrome (HHNS). These life-threatening conditions require immediate medical intervention. (For more information, see Distinguishing between DKA and HHNS, page 252.)
Patients with diabetes mellitus also have a higher risk of various systemic chronic illnesses. The most common chronic complications include cardiovascular and peripheral vascular disease, retinopathy, nephropathy, diabetic dermopathy, and peripheral and autonomic neuropathy. Nearly two-thirds of people with diabetes mellitus die of cardiovascular disease. It’s also the leading cause of renal failure and blindness.
Peripheral neuropathy usually affects the hands and feet and may cause numbness or pain. Autonomic neuropathy manifests itself in several ways, including gastroparesis (leading to delayed gastric emptying and a feeling of nausea and fullness after meals), nocturnal diarrhea, sexual dysfunction, and postural hypotension.
Hyperglycemia impairs the patient’s resistance to infection because the glucose content of the epidermis and urine encourages bacterial growth. The patient is therefore susceptible to skin and urinary tract infections and vaginitis. Patients with diabetes mellitus also have an increased incidence of cognitive depression.
Infants of females with diabetes have a two-to-three-times greater incidence of malformation and fetal distress.
Assessment
The patient with type 1 diabetes usually reports rapidly developing symptoms. With type 2 diabetes, the patient’s symptoms are usually vague and long-standing and develop gradually. Patients with type 2 diabetes generally report a family history of diabetes mellitus, gestational diabetes or the delivery of a baby weighing more than 9 lb, a severe viral infection, autoimmune dysfunction, other endocrine disease, recent stress or trauma, or the use of drugs that increase blood glucose levels.
Patients with either type of diabetes may report symptoms related to hyperglycemia, such as polyuria, polydipsia, polyphagia, weight loss, and fatigue. Or they may complain of weakness; vision changes; frequent skin infections; dry, itchy skin; sexual problems; and vaginal discomfort—all symptoms of diabetes complications.
Inspection may show retinopathy or cataract formation. Skin changes—especially on the legs and feet—indicate impaired peripheral circulation. Muscle wasting and loss of subcutaneous fat may be evident in type 1 diabetes; type 2 is characterized by thin, muscular limbs and fat deposits around the face, neck, and abdomen.
Palpation may detect poor skin turgor and dry mucous membranes related to dehydration. Decreased peripheral pulses, cool skin temperature, and decreased reflexes may also be palpable. Auscultation may reveal orthostatic hypotension. Patients with DKA may have a characteristic “fruity” breath odor because of increased acetone production.