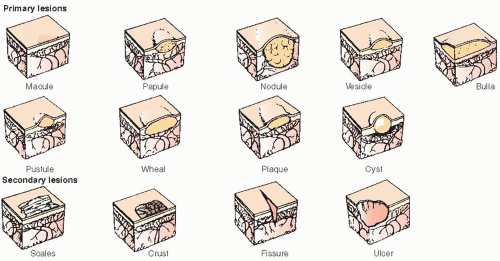
Macule—flat, circumscribed discoloration of skin; may have any size or shape.
Papule—solid, elevated lesion less than 1 cm wide.
Nodule—raised, solid lesion larger than 1 cm wide.
Vesicle—circumscribed elevated lesion less than 0.5 cm, containing fluid.
Bulla—a vesicle or blister larger than 0.5 cm wide.
Pustule—circumscribed raised lesion that contains pus; may form as a result of purulent changes in a vesicle.
Wheal—elevation of the skin that lasts less than 24 hours, caused by edema of the dermis; may be surrounded by erythema or blanching.
Plaque—solid, elevated lesion on the skin or mucous membrane, larger than 1 cm in diameter; psoriasis is commonly manifested as plaques on the skin; leukoplakia is an example of plaques on mucous membranes.
Cyst—soft or firm mass in the skin, filled with semisolid or with liquid material contained in a sac.
Scale—heaped-up, horny layer of dead epidermis; may develop as a result of inflammatory changes.
Crust—covering formed by the drying of serum, blood, or pus on the skin (scab).
Excoriation—linear scratch marks or traumatized areas of skin.
Fissure—linear cracks in the skin, usually from marked drying and long-standing inflammation.
Ulcer—lesion formed by local destruction of the epidermis and by part or all of the underlying dermis.
Lichenification—thickening of skin accompanied by accentuation of skin markings.
Scar/keloid—abnormal new formation of connective tissue that replaces the loss of substance in the dermis as a result of injury or disease. A keloid is a hypertrophic scar that is larger than the original lesion or injury.
Atrophy—diminution in size or in loss of skin cells that causes thinning of the skin.
Petechiae—circumscribed deposits of blood or blood pigment 1 to 2 mm wide.
Purpura—circumscribed deposits of blood or blood pigment greater than 0.5 cm wide.
Comedones—hair follicle obstructed by a sebum and keratin plug; blackheads and whiteheads.
Telangiectasia—small, irregular blood vessels visible in the epidermis.
Burrow—linear, irregular, elevated tunnel produced by parasites in the skin.
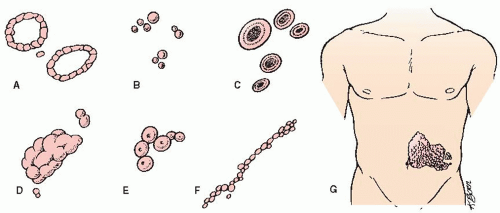
Annular—ring-shaped.
Circinate—circular.
Confluent—lesions run together or join.
Discoid—disk-shaped.
Discrete—lesions remain separate.
Generalized—widespread eruption.
Grouped—clustering of lesions.
Guttate—droplike.
Herpetiform—grouped vesicles.
Iris—ring or a series of concentric circles (bull’s-eye).
Linear—in lines.
Nummular—coin-shaped.
Polymorphous—occurring in several or many forms.
Reticulated—lacelike network.
Serpiginous—snakelike or creeping eruption.
Telangiectatic— a tiny red thread or line.
Zosteriform or dermatomal—bandlike distribution, limited to one or more dermatomes of skin.
When did the rash first occur? Was the onset sudden or gradual?
What site was first affected? Describe the spread and its severity.
What was the initial color and configuration of the rash? Has it changed?
Is there associated itching, burning, tingling, pain, or numbness?
Has it been constant or intermittent?
What makes the rash worse or better? Is it seasonal? Is it affected by stress?
What medications are being taken? What topical products have been used? What effect did they have?
What skin products are used? What chemicals have come into contact with the skin: such as laundry detergent, cleaning products, insecticides, or nickel?
Has there been pet contact?
What is the patient’s occupation? Any hobbies, such as gardening or hiking, that may have contributed? Are latex gloves worn routinely? Is frequent handwashing required?
What is the sexual history and chance of sexually transmitted disease exposure (if relevant)?
Any international travel?
Is there a history of hay fever, asthma, hives, eczema, or allergies?
Has the patient had this particular rash or other skin disorders in the past?
What is the family history of skin disorders?
Are there any long-standing medical problems? Immunosuppressive therapy?
Focus your examination on the skin, hair, and nails. Some dermatologic conditions affect other body systems (eg, hair loss may be associated with thyroid disease or anemia); perform a general physical exam, as indicated.
Ask the patient to show you the area of concern and examine the skin surface under good lighting. Patients should be undressed, in a gown, and the skin of the total body should be examined, not just the area affected.
Note the distribution and configuration of skin lesions. Compare right and left sides of the body.
Note the shape, border, texture, and surface of the lesions.
Palpate the lesions for texture, warmth, and tenderness.
Use a metric ruler to determine size of lesions to serve as a baseline for comparison with subsequent measurements.
Examine the scalp, nails, and oral mucosa.
Perform diascopy—gently press a glass slide or Lucite rule over a skin lesion to detect blanching (caused by dilated blood vessels).
Use a Wood’s light to inspect for fluorescent changes with some fungal infections. Clean skin prior to examination because some ointments, soaps, or deodorant may fluoresce.
For dark-skinned patients look for black, purple, or gray lesions; palpate carefully to determine if rash is present.
Sample taken by scraping, swabbing, or aspirating a lesion is transferred to a glass slide for microscopic examination or staining.
Direct visualization of scrapings mixed with mineral oil to detect scabies, mites, or lice nits that cling to hair.
A Tzanck smear is obtained from vesicular fluid or a moist ulcer and stained to detect characteristics of herpes simplex virus, herpes zoster, and varicella. This is rarely done in the office but properly obtained specimen could be sent to the lab.
Potassium hydroxide may be added to skin scrapings on a glass slide and heated to dissolve skin cells to detect hyphae and spores in fungal infections.
Gram stain may be performed by the lab or dermatopathologist to tentatively identify bacteria or fungi in certain skin infections.
To obtain the specimen for microscopy use the side of a glass slide or a scalpel held at a 45-degree angle to gently scrape the active border of a dry lesion or of an inflamed area; only mild discomfort and pinpoint bleeding should occur.
For moist or semi-moist ulcerations or crusted lesions, roll saline-soaked cotton or Dacron-tipped swab over the lesion; for weeping lesions, use a dry swab.
For intact vesicles, aspirate fluid from the edge with a 25G sterile needle; if vesicle is partially broken, gently unroof with forceps and obtain fluid on a swab.
Drainage from lesions may be cultured on specific media to detect causative organism and sensitivity to antimicrobial therapy; also, portions of skin, hair, and nails may be submitted for fungal culture.
Usually takes 24 to 48 hours for results; fungal cultures may take 4 to 5 weeks.
Obtain specimen with cotton or Dacron-tipped swab and send to laboratory in bacterial culture container clearly labeled with the patient’s name, the date, and the site where the specimen was obtained or in a viral culture container also clearly labeled. Refrigerate viral culture if laboratory pickup is delayed.
To obtain specimen for fungal culture, scrape or clip the affected skin, hair, or nails; then place into a dry, sterile container for transport or onto a dermatophyte test medium.
During your initial visit, which lasts approximately 30 minutes, the nurse will apply one or more small aluminum disks or tape strips to an area on your upper back (used as the test site because the strongest responses are seen in this area). These disks, or patch test kits, contain small amounts of each suspected chemical or allergen; the substances to be tested are determined by your dermatologist or other health care provider. A visible reaction in the skin in contact with a disk indicates allergy to the substance contained in that disk. This redness or rash may itch and persist for several days to several weeks.
You will be advised to return 48 hours later. At this time, the nurse will remove the patches, mark your skin, and do the first reading; you will be expected to remain at the office for 30 minutes so that the nurse can complete the reading.
A final reading will be done on your next visit, which will take place 96 hours to 1 week after the disks have been removed. A copy of your test results will be provided and explained to you at this visit.
DO wear loose or high-necked clothing throughout the day. Wear a T-shirt to bed to avoid catching the edges of the tape on the bed sheets.
DO apply tape to the patch edges if they become loose.
DO contact your health care provider immediately if a patch test area burns severely or if you are unable to carry out normal daily activities. Note: Some itching will occur if you are having a positive reaction; you do not need to call your dermatologist.
DO NOT wet the patches during the testing period—for example, do not take showers. Sponge baths are allowed as long as care is taken to keep the patches completely dry.
DO NOT engage in strenuous activities. Exercise may result in excess sweating, thereby causing the tape to loosen.
DO NOT expose your back to the sun for 2 weeks before patch testing.
DO NOT discontinue antihistamine therapy (these agents do not affect test results).
DO NOT use nonmedicated creams and lotions on your back for at least 24 hours before testing (lotions and creams prevent patches from sticking).
Vesicular disorders, eczema, atopic dermatitis.
Acute inflammatory conditions.
Erosions and exudative, crusted surfaces.
Prepare the bath or teach patient to prepare a lukewarm bath at 90° to 100° F (32.2° to 37.8° C); with the tub half-full, add the prescribed quantity of medication and mix thoroughly to prevent sensitivity reaction. Add oatmeal products or oils to emulsifying baths.
Bleach baths may be used for acute and chronic atopic dermatitis.
Add ½ cup of bleach to full tub or ¼ cup to half tub of warm water and soak limbs and torso for 5 to 10 minutes (do not submerge head), no more than twice a week.
Do not rub the skin. Soaking for at least 5 to 10 minutes will promote removal of loosened scales.
Keep the room and water at comfortable temperatures and limit bathing to 20 to 30 minutes; the bath area should be well ventilated if tars are used because they are volatile.
Tell patient to use a bath mat inside the tub and to use a rug outside the tub when bathing at home because medication may make the tub and other wet surfaces slippery.
Blot skin dry with a towel and apply emollient or topical medication to moist skin. While skin is wet, apply steroid to inflamed areas, if prescribed.
Finn chambers (strips of 10 shallow aluminum cups or chambers 3 inches [8 cm] wide) or TRUE test strip
Allergens (2-inch [5-cm] ribbons of petrolatum-base allergen or disks with filter paper dampened with aqueous solution). Standard tray includes:
Benzocaine 5%
Mercaptobenzothiazole 1%
Colophony 20%
p-Phenylenediamine 1%
Imidazolidinyl urea 2%
Cinnamic aldehyde 1%
Lanolin alcohol 30%
Carba mix 3%
Neomycin sulfate 20%
Thiuram mix 1%
Formaldehyde 1%
Ethylenediamine dihydrochloride 1%
Epoxy resin 1%
Quaternium-15 2%
P-tert-Butylphenol formaldehyde resin 1%
Mercapto mix 1%
Black rubber mix 0.6%
Potassium dichromate 0.25%
Balsam of Peru
Nickel sulfate
| ||||||||||||||||||||||||
Table 33-1. Therapeutic Baths | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||
Bacterial infections that require drainage.
Inflammatory and pruritic conditions.
Oozing and crusting conditions.
Apply dressing to affected area or teach patient to apply. Moisten to the point of slight dripping; remoisten as necessary.
Use warm tap water if warming is desired.
Application may be from 5 to 15 minutes three to four times per day, unless otherwise indicated.
Keep patient warm and do not treat more than one third of body at a time because open wet dressings can cause chilling and hypothermia.
Teach patients to prevent burns by measuring temperature of solution with a bath thermometer or by testing tap water on wrist before applying compress. Advise them not to use microwave ovens to warm dressings because uneven heating can occur.
Wash area and pat dry.
Apply medication while skin is still moist.
Cover with plastic wrap, vinyl gloves, or plastic bag.
Seal with paper tape at edges or cover with other self adhesive dressing to hold in place.
 DRUG ALERT Excessive use of occlusive dressings that contain corticosteroids may cause skin atrophy, striae, telangiectasia, folliculitis, nonhealing ulceration, erythema, and systemic absorption of corticosteroids.
DRUG ALERT Excessive use of occlusive dressings that contain corticosteroids may cause skin atrophy, striae, telangiectasia, folliculitis, nonhealing ulceration, erythema, and systemic absorption of corticosteroids.
Do not apply to ulcerated or abraded skin; removal is recommended within 12 to 24 hours. High-potency steroids are for short-term use only.
Apply dry gauze dressing using clean technique (unless sterile technique is indicated by open wounds).
Wrap extremities with elastic or cotton-rolled bandages or apply tape. Avoid constricting circulation.
Alternative dressing materials can be used for home care, such as disposable or white cotton gloves for the hands, cotton socks for the feet, sheets or towels for large areas, disposable diapers or towels folded in diaper fashion for the groin, washcloths for the axilla, cotton T-shirt or cotton pajamas for the trunk, turban or plastic shower cap for the scalp, or mask made from gauze for the face, with holes cut for the eyes, mouth, and nose.
Shave biopsy—scalpel used to remove raised lesions, leaving lower layers of dermis intact.
Punch biopsy—special instrument used to remove round core of lesion, containing all layers of skin. Biopsy site is usually closed with sutures.
Excisional biopsy—scalpel and scissors used to remove entire lesion, usually with prescribed margins; suturing required.
Position patient comfortably with the site exposed; explain that a local anesthetic will be given. Check if patient has any known allergies to local anesthetics. Ask patient what current medication he or she is taking. Aspirin, some herbal supplements, or anticoagulants may cause increased postoperative bleeding.
Explain the procedure.
Obtain written consent.
After the biopsy, apply hemostatic agent and pressure to the site to stop bleeding, along with an appropriate dressing. Pressure dressing may be required for larger wounds or wounds that are bleeding.
Place the biopsy specimen in a clearly labeled container with 10% formaldehyde and transport it to the dermatopathology lab for hematoxylin and eosin staining. It is essential that skin biopsies be sent to a specialized dermatopathology lab for examination by a dermatopathologist in order to get the best analysis and most complete information on the histology of the skin disease or lesion.
Keep the bandage on surgery site for 24 to 48 hours. During this time, keep site clean and dry.
After this time, remove the bandage and do the following daily:
Wash the incision with soap and water.
Dry the incision well.
Apply petroleum- or mineral oil-based ointment, such as Vaseline or Aquaphor, one to four times per day, keeping the incision moist at all times.
After a few days the dressing is no longer needed, but continue to apply ointment one to four times per day to keep the site moist and help reduce scarring.
Do not apply makeup directly to the stitches.
Repeat wound care for 2 or 3 days after stitches have been removed, unless otherwise instructed.
Use caution when shaving around stitches on face.
 DRUG ALERT
DRUG ALERTand function. These are sometimes used following Mohs micrographic surgery to remove skin cancers, especially on the face, head, and neck.
A section of skin tissue is separated from its blood supply and transferred as free tissue to a distant (recipient) site; it must obtain nourishment from capillaries at the recipient site.
In dermatology, skin grafting is used to repair defects that result from excision of skin tumors and to cover areas of denuded skin.
Definitions.
Autografts—gra\fts done with tissue transplanted from the patient’s own skin.
Allografts—involve the transplant of tissue from one individual of the same species; these grafts are also called allogenic or homografts.
Xenograft or heterograft—involves the transfer of tissue from another species.
Classification by thickness.
Split thickness (thin, intermediate, or thick)—graft that is cut at varying thicknesses and is used to cover large wounds because its total potential donor area is virtually unlimited.
Full thickness—graft consists of epidermis and all of the dermis without the underlying fat; used to cover wounds that are too large to close primarily. They are used frequently to cover facial defects because they provide a better contour match and less postoperative contracture.
A flap is a segment of tissue that has been left attached at one end (called a base or pedicle); the other end has been moved to a recipient area. It is dependent for its survival on functioning arterial and venous blood supplies and on lymphatic drainage in its pedicle or base.
Free flap or free-tissue transfer—one that is completely severed from the body and is transferred to another site; receives early vascular supply from microvascular anastomosis with vessels at recipient site.
Flaps may consist of skin, mucosa, muscle, adipose tissue, and omentum.
Used for wound coverage and to provide bulk, especially when bone, tendon, blood vessels, or nerve tissue are exposed.
Flaps offer the best aesthetic solution because a flap retains the color, texture, and thickness match of the donor area.
Flaps are classified according to the method of movement, composition, location, or function.
Split-thickness skin graft is obtained by razor blade, skingrafting knife, or electric or air-powered dermatome or drum dermatome. Most commonly obtained from the inner aspect of the upper arm or outer thigh.
A full-thickness skin graft is primarily excised, defatted, and tailored to fit accurately over the defect area.
Skin is taken from the donor or host site and applied to the wound or defect site, called the recipient site or graft bed.
A bolster (pressure) dressing is applied to the graft to enhance the survival of the skin graft by providing stable approximation of the graft to the recipient bed.
The bolster dressing is left in place for 1 week. The process of revascularization and reattachment of the skin graft to the recipient bed is referred to as a take.
The donor site is maintained clean and dry.
If Scarlet Red (a single layer dressing impregnated with epithelial growth promoter) is used on the donor site for split-thickness grafts, it is left in place for 2 to 3 weeks to allow the wound to heal.
Occlusive dressings, such as Omniderm or Allevyn, may also be used to decrease pain, alleviate frequent wound care, and speed healing.
Daily wound care and dressing change with an antimicrobial ointment and nonstick dressing may also be used.
 NURSING ALERT
NURSING ALERT
Aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) and vitamin E are discontinued 14 days before the procedure. Coumadin should be held for several days before the procedure, and prothrombin time and International Normalized Ratio should be measured before the procedure, as ordered. Herbal supplements, such as ginkgo, ginseng, green tea, and vitamin E, can inhibit coagulation.
Efforts should be made to enhance wound healing several months to several weeks before the procedure, such as smoking cessation, alcohol avoidance, and proper nutrition.
Medical history and examination should be evaluated, particularly for latex sensitivity, cardiovascular problems requiring endocarditis antibiotic prophylaxis, bleeding problems, and high blood pressure (BP).
The procedure is usually done under local anesthetic, so no meals are withheld.
The operative site should be free from makeup.
The patient should have someone available to drive him or her home after surgery unless otherwise notified.
Initial pressure dressing will be left in place for 24 to 48 hours.
If wound begins to ooze, apply firm pressure for 10 to 15 minutes (without peeking). If bleeding persists, contact surgeon.
Do not take aspirin or aspirin-containing medication for pain. May take one to two acetaminophen tablets every 4 to 6 hours, as needed.
Most skin grafts are held in place by a bolster dressing (cotton ball or foam). Do not remove the bolster dressing during the next week.
May clean site and apply ointment to the surrounding area of the bolster dressing.
Do not get the bolster dressing wet.
When the bolster dressing is removed, may shower, but do not let the water hit the graft directly.
Keep the graft edges moist with ointment.
Protect the graft from the sun. The sun will cause pigmentation changes in the graft. A sunscreen may be used in 2 to 3 weeks.
Skin grafts to the lower leg must be kept elevated because the new capillary connections are fragile and excess venous pressure may cause rupture. Keep leg elevated as much as possible during the next week.
Inspect the dressing daily. Report unusual drainage or signs of an inflammatory reaction.
After 2 to 3 weeks, any water-based moisturizer may be applied to the skin donor site for split-thickness skin grafts.
Expect some loss of sensation in the grafted area for a time.
Avoid strenuous exercise (jogging, lifting heavy objects). Anything that causes face flushing will raise BP, cause bleeding, and impair healing.
Done through various techniques and incisions to alleviate skin folds and wrinkles to improve the appearance of the aging face (face lift).
The correction can last as long as 10 years, but results vary with each individual. Skin relaxes with time and the muscles may also relax, but seldom does the face revert to its preoperative condition.
Surgical procedures include:
Operative: Standard incisions that are either temporal (hidden in hairline) or submental.
Laser: Several laser modalities are now used in facial plastic surgery, including radio-frequency tissue tightening, which causes collagen shrinkage and reduction of deep wrinkles and lines.
Removes loose skin, muscle, and excess fat from upper or lower eyelids. It will not remove lines at the lateral corners of the eyes (“crow’s feet”).
The procedure is generally done by either scalpel under local or general anesthetic or by carbon dioxide laser.
Patients with weathered skin, fine wrinkles (especially at the corners of the eyes and along the vermilion border), or acne pitting and scarring may benefit from these procedures.
The use of laser technology allows for a more predictable result and eliminates the porcelain appearance resulting from such chemicals as trichloroacetic acid. There is less risk of hypopigmentation than with dermabrasion.
Chemical peels using tretinoin cream and alpha-hydroxy acids result in the destruction of portions of the epidermis and dermis, with subsequent regeneration of new tissues.
New nonablative laser resurfacing is used for fine wrinkles, smoker lines, sun-damaged skin, and shallow acne scarring with minimal downtime.
Contraindications of laser resurfacing include:
History of isotretinoin therapy 6 to 12 months prior to treatment.
Status of postradiation or scleroderma.
History of herpes simplex—requires perioperative treatment.
Hyperpigmentation can occur in persons with dark skin.
Purified botulinum toxin and fillers (collagen, hyaluronic acid, autologous fat) are used to correct deep wrinkles and facial hollows. Results may last 3 to 12 months.
Also called body contouring, liposuction reduces localized deposits of fat not amenable to weight loss with a cannula aided by suction or fitted to a syringe.
May be done on the face, neck, breasts, abdomen, flanks, hips, buttocks, and extremities.
Local or general anesthetic will be administered. For local anesthetic, patient may eat and drink before surgery. For general anesthetic:
Preoperative assessment may be necessary, depending on health status and patient’s age.
No eating or drinking for several hours before surgery.
Patient should have escort and must be reminded not to drive home alone after surgery.
Review patient’s allergies and medication before surgery.
Instruct patient to cleanse skin with antiseptic agent the night before surgery, if prescribed.
Make sure patient thoroughly understands the procedure and has discussed the risks and benefits with the health care provider before surgery.
Make sure a consent form is signed before any procedure.
Make sure aspirin, warfarin, and NSAIDs have been discontinued for 2 weeks before surgery, unless otherwise indicated. Herbal supplements, such as ginkgo, ginseng, green tea, and vitamin E, can inhibit coagulation.
If applicable, instruct the patient to stop smoking for the 2 weeks leading up to rhytidectomy and to continue cessation for 2 weeks postprocedure and permanently, if possible.
Be aware of signs of topical lidocaine toxicity (if used)— drowsiness, tingling of lips, metallic taste—which may lead to seizures.
Mild exercise can be resumed in 3 days postoperatively.
No strenuous exercise (that will increase the BP) for 1 month.
Dressings are usually removed on the first postoperative day. Elastic facial support garment is recommended for 1 to 3 weeks.
Eyelid sutures are removed in 3 to 5 days; facial sutures in 7 days.
Showering and gentle hair washing may begin on day 2 or 3.
The patient is to apply ointment (petroleum or a similar ointment) to all suture lines.
Stress to the patient not to remove crusts by “picking” at them along suture lines or scarring may result.
Elevate the head at night for 2 weeks after the procedure. Avoid bending and lifting, which may increase edema and provoke bleeding.
Expect the face or affected part to be swollen, bruised, and numb for several days to weeks.
Be aware that complications include bleeding and hematoma, sloughing of skin, and possible facial nerve damage. Notify surgeon if the areas become increasingly red or swollen or if they become more tender or painful.
Apply iced gauze compresses to eyes for 10 minutes four to six times per day to reduce edema after surgery.
Head of bed should be elevated to reduce internal pressure that might cause bleeding.
Avoid strenuous exercise for 1 week.
Bruising and swelling generally resolve in 2 weeks.
Watch for such complications as eyelid hematomas, ocular mobility dysfunction, and postsurgical ectropion (eversion of the edge of the eyelid).
Instruct patients to not pick at crusts because new epithelium will be injured; soak face several times per day and apply emollient, as directed. Crusts form in 2 to 3 days and start to separate by 7 to 10 weeks. Total separation can take up to 3 weeks.
Keep treated areas clean and moist.
Avoid sun on treated areas. Apply sunscreen with sun protection factor (SPF) of 15 to 30 when outdoors.
Manage bruising and swelling from injectables with ice packs.