Cryosurgery
Often performed in the physician’s office, cryosurgery refers to the destruction of tissue by the application of extreme cold. The procedure is used to treat such dermatologic conditions as actinic and seborrheic keratoses, leukoplakia, molluscum contagiosum, condyloma acuminatum, verrucae and, sometimes, early basal cell epitheliomas and squamous cell carcinomas. It’s also used to treat gynecologic conditions, such as cervicitis, chronic cervical erosion, cervical polyps, and condyloma acuminata, as well as ophthalmic conditions, such as cataracts and retinal tears or holes.
Cryosurgery’s success depends on the type of lesion, the extent and depth of the freeze, and the duration between freezing and thawing. A slow thaw destroys lesions most effectively. Liquid nitrogen and nitrous oxide (N2O) are the most commonly used cryogens. Carbon dioxide and freon are less frequently used. At -320° F (-196° C), liquid nitrogen is by far the most powerful cryogen. It’s especially useful for treating cancers, which resist cold well because of their vascularity. N2O is often favored for less extensive procedures, since the surgeon can more easily control its effects.
More convenient versions, such as dimethylester propiane spray at -67° F (-55° C), are available for use in medical offices and clinics; however, use of these agents is restricted to warts and benign skin lesions, and their function is similar to that of N2O models.
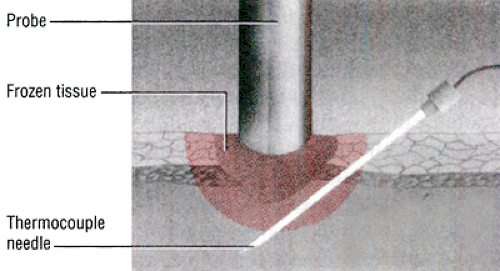
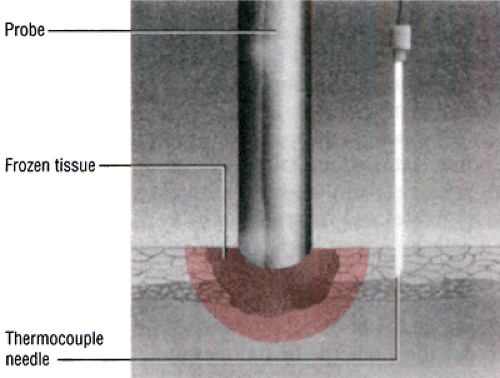
Positioning thermocouple needles
During cryosurgery, you may be responsible for positioning thermocouple needles and then operating them according to the surgeon’s direction. These needles measure the temperature of the tissue at its tip and help the physician gauge the depth of freezing—a vitally important factor when destroying cancerous lesions. The needle may be placed in any of several positions.
Precise temperature measurement can be difficult because a variation of only 1 mm in the needle’s position can translate into a difference of 50° to 59° F (10° to 15° C). For that reason, you’ll usually place two or more needles in different areas to increase the accuracy of the reading.
In this illustration, the needle is shown inserted at an angle so that its tip rests about 5 mm below the base of the tumor to give a direct reading of tissue temperature. In this position, the temperature reading may be affected by chilling of the shaft within the frozen tissue, but the error isn’t likely to be significant.
Here the probe is placed about 5 mm to one side of the frozen tissue at a depth of about 3 mm. In this position, it will register the same temperature as the probe above because both probe tips are about the same distance from the frozen tissue.
Procedure
The procedure varies with the area being treated. For dermatologic cryosurgery, the surgeon may give a local anesthetic, depending on the type and extensiveness of the lesion. He’ll then determine the correct temperature and depth for freezing. For superficial lesions, he can often determine this simply by palpating and observing the lesion. For skin cancers, however, he’ll use thermocouple needles and a tissue temperature monitor (pyrometer) to be sure that tissue at the deepest part of the lesion has been adequately frozen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree