Musculoskeletal pain—characteristics.
Joint swelling.
Morning stiffness.
Constitutional symptoms.
Fever.
Weight loss, anorexia.
Fatigue.
Involvement of other body symptoms.
Skin.
Ocular.
Pulmonary.
Neurologic.
Mucous membranes.
Gastrointestinal (GI).
Depression or psychosis.
Self-care activities and functional ability.
Social activities and roles.
Family history of rheumatic or autoimmune disorders.
Musculoskeletal examination:
Pain on palpation or range of motion (ROM).
Joint swelling, warmth, or erythema.
Joint motion restriction.
Pain, swelling, or warmth of soft tissues surrounding joints.
Deformities.
Skin:
Skin rash or other abnormalities such as thickening.
Alopecia.
Oral mucosa:
Ulcerations.
Dryness.
Ocular:
Conjunctival inflammation.
Dryness.
Pulmonary:
Adventitious sounds.
Friction rub.
Neurologic:
Foot drop.
Muscle weakness.
Neurologic deficits.
High anti-dsDNA levels are associated with the development of lupus nephritis.
There is a low false-positive rate (about 5%) in patients with other connective tissue disorders; in patients taking medications such as minocycline, etanercept, infliximab, and penicillamine; in first-degree relatives of patients with lupus; and in some laboratory workers.
There is no special preparation for this blood test.
Anti-CCP is about as sensitive, but more specific (95% to 98%), than the rheumatoid factor test. Found in approximately 50% to 55% of patients with RA.
It may be valuable in cases of early arthritis when symptoms are mild and nonspecific and aggressive treatment is being contemplated. Anti-CCP antibody is now used with the rheumatoid factor as the gold standard in making the diagnosis of rheumatoid arthritis.
Some laboratories are currently doing a second generation of the test—the CCP2 assay.
No specific preparation is needed for this blood test, but the specimen may need to be sent out for processing, as not all labs perform this test.
Be alert for drugs that may cause false-positive results.
Table 30-1 ANA Staining Patterns and Connective Tissue Disorders
ANA PATTERN
CONNECTIVE TISSUE DISORDER
Peripheral (rim, ring, membranous)
Active SLE, usually with renal disease
Homogenous (diffuse)
SLE, RA
Speckled
SLE, RA, scleroderma, Sjögren’s syndrome, mixed connective tissue disorder
Nucleolar
Scleroderma
ANA, antinuclear antibody; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus.
Results will be reported in a staining pattern (speckled, homogeneous, peripheral, nucleolar) if positive, which correlates to various types of connective tissue disorders and various subsets of SLE (see Table 30-1).
Titer will also be reported with positive ANA but does not reflect disease activity or prognosis.
Complement is a complex cascade system that activates proteins as part of the body’s defense against infection.
Specific components include CH50 (total complement), C3, and C4; measurement helps determine immune complex formation or agammaglobulinemia.
Complement levels are decreased in certain autoimmune diseases, particularly SLE, because of complement consumption and because of activation of proteolytic enzymes and tissue damage. C3 and C4 are often monitored to evaluate activity in SLE.
Obtain venous blood sample and refrigerate; send to laboratory promptly because complement deteriorates at room temperature.
Serial measurements may be helpful in monitoring the activity of some rheumatic diseases; decreased levels indicate increased disease activity.
CRP reacts quicker to inflammatory changes than erythrocyte sedimentation rate; it rises within a few hours of an infection or inflammatory condition and then decreases quickly when inflammation resolves.
CRP can be used to differentiate inflammatory from noninflammatory conditions and to monitor effectiveness of treatment.
Normal CRP is usually below 10 mg/L; a level over 100 mg/L usually indicates infection or inflammation; however, some inflammatory conditions can raise CRP a thousandfold.
Table 30-2 Synovial Fluid Analysis | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Erythrocyte sedimentation rate (ESR) determines the rate at which red blood cells (RBCs) fall out of unclotted blood in 1 hour.
The test is based on the premise that inflammatory and other disease processes create changes in blood proteins, thus causing aggregation of RBCs that makes them heavier.
ESR is generally elevated in most rheumatic illnesses.
The test is sensitive for inflammatory condition, but not specific to connective tissue disorders.
Result may be elevated by pregnancy, menstruation, medications (such as heparin and oral contraceptives), infection, malignancy, anemia, and advanced age.
Result may be reduced by elevated blood glucose or albumin, high phospholipids, or drugs, such as corticosteroids or high-dose aspirin.
Most beneficial in monitoring inflammatory disease.
It is not a highly sensitive or specific test.
May be positive in 50% to 75% of patients with RA, SLE, and Sjögren’s syndrome. May be false-positive with endocarditis, tuberculosis, syphilis, sarcoidosis, cancer, viral infections, hepatitis C, patients with skin or renal allographs, and in some liver, lung, or kidney diseases.
Negative RF does not exclude the diagnosis of RA.
Certain disease manifestations, such as severe joint involvement and extra-articular manifestations, may be more frequent in those with high-titer RF.
A sample of synovial (joint) fluid is analyzed for several components.
Color.
Clarity/turbidity.
Viscosity.
White blood cell (WBC) count with differential.
Crystals and their identification.
Arthrocentesis, a sterile procedure, requires antiseptic cleaning agent, local anesthetic, a 20G needle (an 18G needle if infected fluid is suspected), and a 10- to 20-mL syringe.
Patients are generally apprehensive about having a needle inserted into a joint. They require reassurance and explanation of the importance of information derived from test results.
Assist the health care provider with the test by collecting supplies, maintaining a sterile field, sending joint fluid samples for testing, and monitoring for bleeding following the procedure.
Results help to differentiate infection, inflammation, and crystal deposition in a painful joint (see Table 30-2).
 Evidence Base
Evidence Baseof Arthrtitis and Musculoskeletal and Skin Disease (www.niams.nih.gov/Health_Info/default.asp) or from the American College of Rheumatology. (ACR; www.rheumatology.org).
Table 30-3 Drug Therapy for Connective Tissue Disorders | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Joint conservation.
Energy conservation.
Splinting (in rare instances).
ROM exercises.
Application of heat and cold.
Endurance or aerobic conditioning.
Modification of home and work environment.
Perform activities using good body mechanics.
Maintain ideal body weight—extra weight places undue stress on weight-bearing joints.
Use large joints to perform activities—spread the load over as many joints as possible.
Perform activities in smooth movements to avoid trauma induced by abrupt movements.
Organize materials, utensils, and tools.
Perform lengthy activities in a seated position.
Work at an even pace—avoid rushing.
Delegate work to others when possible.
May be used for wrists and hands.
Ensure proper application.
Periodically inspect for skin irritation, neurovascular compromise, or improper fit.
Usually worn during acute stage of inflammation to protect joint.
Avoid exercising inflamed joints—putting these joints through ROM exercises one to two times per day when inflamed is sufficient.
Perform exercises daily, as prescribed.
Aerobic conditioning exercises may be indicated when disease activity permits.
Walking, biking, swimming, and water walking for 30 minutes, three times per week. Regular exercise three times per week for at least 20 minutes for 6 months has been shown to reduce fatigue and disability in patients with RA compared to those who didn’t exercise.
Reinforce correct use and application of heat and cold.
Obtain and teach correct use of assistive devices.
Reinforce use of behavior-modification and relaxation techniques as adjuncts to therapy.
Suggest discussion with health care provider about complementary and alternative therapies. A wide variety of herbal and nutraceutical products have been used and studied, but data remain inconclusive about efficacy (see Table 30-4).
Many herbal and supplemental products are marketed for pain, inflammation, repair of cartilage, and boosting the immune system; however, scientific evidence for clear-cut treatment benefit is lacking. There is preliminary evidence for fish oil, gamma-linolenic acid, and the herb thunder god vine.
Table 30-4 Complementary and Alternative Drug Therapy for Arthritis
DRUG AND EFFECT
EFFECT
COMMENTS
Fish oil (omega-3 fatty acid)
May reduce tenderness and stiffness; may reduce the need for NSAIDs.
May interact with blood thinners, antihypertensives. Avoid high-dose fish liver oil, which may cause vitamin A and D toxicity.
Gamma-linoleic acid (GLA) (omega-6 fatty acid, evening primrose oil, borage, black currant)
Converted into substances that reduce inflammation to relieve joint pain, stiffness, tenderness, and possibly NSAID use.
Appears to be safe but some borage oil preparations contain hepatotoxic chemicals. More research on dose and duration is needed.
Thunder god vine (Tripterygium wilfordii)
May fight inflammation and suppress the immune system; may relieve rheumatoid arthritis symptoms.
May cause serious side effects—diarrhea, stomach upset, hair loss, headache, skin rash, menstrual changes, male infertility; long-term use may reduce bone mineral density.
Boswellia
Anti-inflammatory and analgesic effects.
Generally safe. Lab and animal studies have been done; need clinical studies.
Ginger
Anti-inflammatory and analgesic effects.
Large doses may cause GI adverse effects; may cause bleeding if given with anticoagulant. Lab studies have been done, need clinical studies.
Green tea
Substances might be useful in rheumatoid arthritis and osteoarthritis.
More information is needed.
Turmeric (curcumin)
Animal studies show protection of joints from inflammation and damage.
Generally safe, no adverse effects; however, may cause stomach ulcers in high doses with prolonged use. Animal studies have been done, need clinical studies.
Cayenne pepper (capsicum)
Thought to deplete substance P, reducing pain transmission
Applied topically to skin over joints in concentrations of 0.025%-0.25%
Takes several days to obtain pain relief; do not use with heat application.
Glucosamine and chondroitin
Cartilage repair, pain relief
Glucosamine: 1,000-2,000 mg daily Chondroitin: 800-1,600 mg daily, based on weight
Bleeding risk if ASA taken with chondroitin; may be effective either alone or as combination; must be taken for several months to achieve noticeable effect. Studies showed conflicting results.
GLA, gamma-linoleic acid.
Reflexology, tai chi, and acupressure or acupuncture have benefited some patients with arthritis and connective tissue disorders. Assist the patient in finding certified providers in these disciplines, if desired.
Use of magnets to relieve pain has not shown effectiveness in numerous studies since the concept was introduced.
For more information, refer patients to the National Center for Complimentary and Alternative Medicine at http://nccam.nih.gov/health/RA/getthefacts.htm.
Advise patient to modify home and work environments, as needed, to install safety devices, and to maintain a safe environment.
Advise patient to seek counseling regarding sexuality if joint pain and inflammation are barriers to performance.
Reinforce the chronic waxing-and-waning nature of the illness to lessen susceptibility to quackery.
 Evidence Base
Evidence Base Evidence Base
Evidence Base Evidence Base
Evidence Base
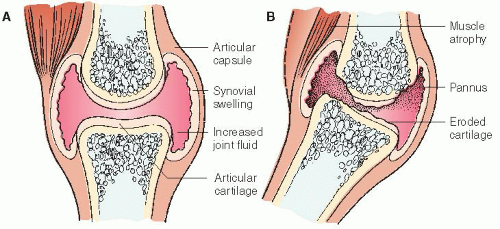
Immunologic processes result in inflammation of synovium, producing antigens and inflammatory by-products that lead to destruction of articular cartilage, edema, and production of a granular tissue called pannus (see Figure 30-1).
Granulation tissue forms adhesions that lead to decreased joint mobility.
Similar adhesions can occur in supporting structures, such as ligaments and tendons, and cause contractures and ruptures that further affect joint structure and mobility.
The etiology is unknown but is probably a combined effect of environmental, epidemiologic, infectious, and genetic factors.
An infectious agent has not been identified, but many infectious processes can produce a polyarthritis similar to RA.
Women are affected more frequently than men.
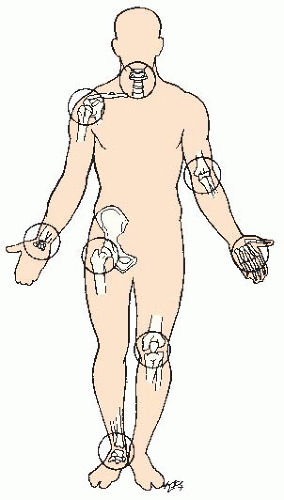
Arthritis-2010 criteria includes synovitis in any joint, rather than symmetrical joints in the 1987 ACR criteria (see Figure 30-2, page 1062).
Skin manifestations.
Rheumatoid nodules—elbows, occiput, sacrum.
Vasculitic changes—brown, splinterlike lesions in fingers or nail folds.
Cardiac manifestations.
Acute pericarditis.
Conduction defects.
Valvular insufficiency.
Coronary arteritis.
Cardiac tamponade—rare.
Myocardial infarction, sudden death—rare.
Pulmonary manifestations.
Asymptomatic pulmonary disease.
Pleural effusion, pleurisy.
Interstitial fibrosis.
Laryngeal obstruction caused by involvement of the cricoarytenoid joint—rare.
Pulmonary nodules.
Neurologic manifestations.
Mononeuritis multiplex—wrist drop, foot drop.
Carpal tunnel syndrome.
Compression of spinal nerve roots.
Distal sensory neuropathy.
Other manifestations.
Fever.
Fatigue.
Weight loss.
Episcleritis.
Complete blood count (CBC)—normochromic, normocytic anemia of chronic disease; may also have iron-deficiency anemia (hypochromic, microcytic); platelets may be elevated with inflammation.
RF—positive in up to 70% to 80% of patients with RA; CCP is more specific for RA than RF testing.
ESR and CRP—often elevated due to active inflammation.
Synovial fluid analysis—see Table 30-2, page 1057.
X-rays—changes develop within 2 years.
Hands/wrists—marginal erosions of the proximal interphalangeal (PIP), metacarpophalangeal, and carpal joints; generalized osteopenia.
Cervical spine—erosions that produce atlantoaxial subluxation (generally after many years).
Magnetic resonance imaging (MRI)—detects spinal cord compression that results from C1 to C2 subluxation and compression of surrounding vascular structures. Also detects erosions earlier then x-ray.
Bone scan—increased uptake in the joints involved in RA.
Ultrasound—detects synovitis and erosion (very user dependent). Musculoskeletal ultrasound is widely used in Europe, but more sporadic use in United States.
Synovial biopsy.
Inflammatory cells associated with RA.
Excludes other causes of polyarthritis by noting the lack of other pathologic findings, such as crystals.
 Evidence Base
Evidence Base
NSAIDs to relieve pain and inflammation.
DMARDs to reduce disease activity.
Monotherapy or combination of older agent, such as methotrexate or hydroxychloroquine, with newer agent, such as tumor necrosis factor (TNF) inhibitor or other biologic agents.
Combination of TNF inhibitor and methotrexate has shown greater benefit in improving signs and symptoms, preventing radiologic deterioration of the joint, and improving physical function in comparison with monotherapy.
Goal is to have long-term impact on the joints and to prevent disability.
Corticosteroids (by mouth or intra-articular administration) to reduce inflammatory process. Generally used for short periods, due to multiple side effects.
Local comfort measures:
Application of heat and cold did not show benefit in a meta-analysis, but treatment can be individualized.
Use of splints to support painful, swollen joints.
Use of transcutaneous electrical nerve stimulation (TENS) unit for 15 minutes three times a week may provide some benefit.
Iontophoresis—delivery of medication through the skin using direct electrical current.
Parrafin wax baths with exercise may be of some benefit.
Nonpharmacologic modalities:
Behavior modification.
Relaxation techniques.
Surgery:
Synovectomy.
Arthrodesis—joint fusion.
Total joint replacement.
 DRUG ALERT
DRUG ALERTStay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree