Conception and Fetal Development
In this chapter, you’ll learn:
anatomic structures and functions of the male and female reproductive systems
effects of hormone production on sexual development
the process of fertilization
stages of fetal development
structural changes that result from pregnancy.
A look at conception and fetal development
Development of a functioning human being from a fertilized ovum involves a complex process of cell division, differentiation, and organization. Development begins with the union of spermatozoon and ovum (conception) to form a composite cell containing chromosomes from both parents. This composite cell (called a zygote) divides repeatedly. Finally, groups of differentiated cells organize into complex structures, such as the brain, spinal cord, liver, kidneys, and other organs that function as integrated units.
|
To fully understand the dramatic physical changes that occur during pregnancy, you must be familiar with reproductive anatomy and physiology and the stages of fetal development. Let’s start with the male reproductive system.
Male reproductive system
Anatomically, the main distinction between a male and a female is the presence of conspicuous external genitalia in the male. In contrast, the major reproductive organs of the female lie within the pelvic cavity.
|
Making introductions
The male reproductive system consists of the organs that produce, transfer, and introduce mature sperm into the female reproductive tract where fertilization occurs. (See Structures of the male reproductive system, page 30.)
Multitasking
In addition to supplying male sex cells (spermatogenesis), the male reproductive system plays a part in the secretion of male sex hormones.
Penis
The organ of copulation, the penis deposits sperm in the female reproductive tract and acts as the terminal duct for the urinary tract. The penis also serves as the means for urine elimination. It consists of an attached root, a free shaft, and an enlarged tip.
What’s inside
Internally, the cylinder-shaped penile shaft consists of three columns of erectile tissue bound together by heavy fibrous tissue. Two corpora cavernosa form the major part of the penis. On the underside, the corpus spongiosum encases the urethra. Its enlarged proximal end forms the bulb of the penis.
The glans penis, at the distal end of the shaft, is a cone-shaped structure formed from the corpus spongiosum. Its lateral margin forms a ridge of tissue known as the corona. The glans penis is highly sensitive to sexual stimulation.
What’s outside
Thin, loose skin covers the penile shaft. The urethral meatus opens through the glans to allow urination and ejaculation.
In a different vein
The penis receives blood through the internal pudendal artery. Blood then flows into the corpora cavernosa through the penile artery. Venous blood returns through the internal iliac vein to the vena cava.
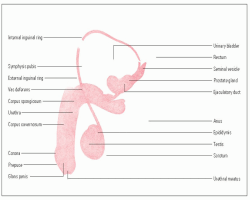
Structures of the male reproductive system
The male reproductive system consists of the penis, the scrotum and its contents, the prostate gland, and the inguinal structures.
|
Scrotum
The penis meets the scrotum, or scrotal sac, at the penoscrotal junction. Located posterior to the penis and anterior to the anus, the scrotum is an extra-abdominal pouch that consists of a thin layer of skin overlying a tighter, musclelike layer. This musclelike layer, in turn, overlies the tunica vaginalis, a serous membrane that covers the internal scrotal cavity.
Canals and rings
Internally, a septum divides the scrotum into two sacs, which each contain a testis, an epididymis, and a spermatic cord. The spermatic cord is a connective tissue sheath that encases autonomic
nerve fibers, blood vessels, lymph vessels, and the vas deferens (also called the ductus deferens).
nerve fibers, blood vessels, lymph vessels, and the vas deferens (also called the ductus deferens).
The spermatic cord travels from the testis through the inguinal canal, exiting the scrotum through the external inguinal ring and entering the abdominal cavity through the internal inguinal ring. The inguinal canal lies between the two rings.
|
Loads of nodes
Lymph nodes from the penis, scrotal surface, and anus drain into the inguinal lymph nodes. Lymph nodes from the testes drain into the lateral aortic and pre-aortic lymph nodes in the abdomen.
Testes
The testes are enveloped in two layers of connective tissue called the tunica vaginalis (outer layer) and the tunica albuginea (inner layer). Extensions of the tunica albuginea separate the testes into lobules. Each lobule contains one to four seminiferous tubules, small tubes where spermatogenesis takes place.
Climate control
Spermatozoa development requires a temperature lower than that of the rest of the body. The dartos muscle, a smooth muscle in the superficial fasciae, causes scrotal skin to wrinkle, which helps regulate temperature. The cremaster muscle, rising from the internal oblique muscle, helps to govern temperature by elevating the testes.
Duct system
The male reproductive duct system, consisting of the epididymis, vas deferens, and urethra, conveys sperm from the testes to the ejaculatory ducts near the bladder.
Swimmers, take your mark!
The epididymis is a coiled tube that’s located superior to and along the posterior border of the testis. During ejaculation, smooth muscle in the epididymis contracts, ejecting spermatozoa into the vas deferens.
|
Descending tunnel
The vas deferens leads from the testes to the abdominal cavity, extends upward through the inguinal canal, arches over the urethra, and descends behind
the bladder. Its enlarged portion, called the ampulla, merges with the duct of the seminal vesicle to form the short ejaculatory duct. After passing through the prostate gland, the vas deferens joins with the urethra.
the bladder. Its enlarged portion, called the ampulla, merges with the duct of the seminal vesicle to form the short ejaculatory duct. After passing through the prostate gland, the vas deferens joins with the urethra.
Tube to the outside
A small tube leading from the floor of the bladder to the exterior, the urethra consists of three parts:
Accessory reproductive glands
The accessory reproductive glands, which produce most of the semen, include the seminal vesicles, bulbourethral glands (Cowper glands), and prostate gland.
A pair of pairs
The seminal vesicles are paired sacs at the base of the bladder. The bulbourethral glands, also paired, are located inferior to the prostate.
Improving the odds
The walnut-size prostate gland lies under the bladder and surrounds the urethra. It consists of three lobes: the left and right lateral lobes and the median lobe.
The prostate gland continuously secretes prostatic fluid, a thin, milky, alkaline fluid. During sexual activity, prostatic fluid adds volume to semen. It also enhances sperm motility and improves the odds of conception by neutralizing the acidity of the man’s urethra and the woman’s vagina.
Basically basic
Semen is a viscous, white secretion with a slightly alkaline pH (7.8 to 8) that consists of spermatozoa and accessory gland secretions. The seminal vesicles produce roughly 60% of the fluid portion of semen, whereas the prostate gland produces about 30%. A viscid fluid secreted by the bulbourethral glands also becomes part of semen.
Spermatogenesis
Sperm formation (also called spermatogenesis) begins when a male reaches puberty and usually continues throughout life.
 Memory jogger
Memory joggerTo remember the meaning of spermatogenesis, keep in mind that genesis means “beginning” or “new.” Therefore, spermatogenesis means beginning of new sperm.
Divide and conquer
Spermatogenesis occurs in four stages:
 In the first stage, the primary germinal epithelial cells, called spermatogonia, grow and develop into primary spermatocytes. Both spermatogonia and primary spermatocytes contain 46 chromosomes, consisting of 44 autosomes and the two sex chromosomes, × and Y.
In the first stage, the primary germinal epithelial cells, called spermatogonia, grow and develop into primary spermatocytes. Both spermatogonia and primary spermatocytes contain 46 chromosomes, consisting of 44 autosomes and the two sex chromosomes, × and Y. Next, primary spermatocytes divide to form secondary spermatocytes. No new chromosomes are formed in this stage; the pairs only divide. Each secondary spermatocyte contains one-half of the number of autosomes, 22; one secondary spermatocyte contains an × chromosome; the other, a Y chromosome.
Next, primary spermatocytes divide to form secondary spermatocytes. No new chromosomes are formed in this stage; the pairs only divide. Each secondary spermatocyte contains one-half of the number of autosomes, 22; one secondary spermatocyte contains an × chromosome; the other, a Y chromosome. In the third stage, each secondary spermatocyte divides again to form spermatids (also called spermatoblasts).
In the third stage, each secondary spermatocyte divides again to form spermatids (also called spermatoblasts). Finally, the spermatids undergo a series of structural changes that transform them into mature spermatozoa or sperm. Each spermatozoa has a head, neck, body, and tail. The head contains the nucleus; the tail, a large amount of adenosine triphosphate, which provides energy for sperm motility.
Finally, the spermatids undergo a series of structural changes that transform them into mature spermatozoa or sperm. Each spermatozoa has a head, neck, body, and tail. The head contains the nucleus; the tail, a large amount of adenosine triphosphate, which provides energy for sperm motility.
|
Queuing up
Newly mature sperm pass from the seminiferous tubules through the vasa recta into the epididymis. Only a small number of sperm can be stored in the epididymis. Most of them move into the vas deferens, where they’re stored until sexual stimulation triggers emission.
Check the expiration date?
After ejaculation, sperm can survive for 24 to 72 hours at body temperature. Sperm cells retain their potency and can survive for up to 4 days in the female reproductive tract.
Hormonal control and sexual development
Androgens (male sex hormones) are produced in the testes and adrenal glands. Androgens are responsible for the development of male sex organs and secondary sex characteristics. One major androgen is testosterone.
|
Team captain
Leydig cells, located in the testes between the seminiferous tubules, secrete testosterone, the most significant male sex hormone. Testosterone is responsible for the development and maintenance of male sex organs and secondary sex characteristics, such as facial hair and vocal cord thickness. Testosterone is also required for spermatogenesis.
Calling the plays
Testosterone secretion begins approximately 2 months after conception, when the release of chorionic gonadotropins from the placenta stimulates Leydig cells in the male fetus. The presence of testosterone directly affects sexual differentiation in the fetus. With testosterone, fetal genitalia develop into a penis, scrotum, and testes; without testosterone, genitalia develop into a clitoris, vagina, and other female organs.
During the last 2 months of gestation, testosterone usually causes the testes to descend into the scrotum. If the testes don’t descend after birth, exogenous testosterone may correct the problem.
Other key players
Other hormones also affect male sexuality. Two of these, luteinizing hormone (LH)—also called interstitial cell-stimulating hormone—and follicle-stimulating hormone (FSH), directly affect secretion of testosterone.
Waiting on the bench
During early childhood, a boy doesn’t secrete gonadotropins and thus has little circulating testosterone. Secretion of gonadotropins from the pituitary gland, which usually occurs between ages 11 and 14, marks the onset of puberty. These pituitary gonadotropins stimulate testis functioning as well as testosterone secretion.
Put me in, coach!
During puberty, the penis and testes enlarge and the male reaches full adult sexual and reproductive capability. Puberty also marks the development of male secondary sexual characteristics, including:
Star player
After a male achieves full physical maturity, usually by age 20, sexual and reproductive function remain fairly consistent throughout life.
Subtle changes
With aging, a man may experience subtle changes in sexual function but he doesn’t lose the ability to reproduce. For example, an elderly man may require more time to achieve an erection, experience less firm erections, and have reduced ejaculatory volume. After ejaculation, he may take longer to regain an erection.
|
Female reproductive system
Unlike the male reproductive system, the female system is largely internal, housed within the pelvic cavity.
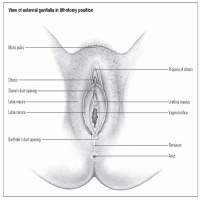
External genitalia
The external female genitalia, or vulva, include the mons pubis, labia majora, labia minora, clitoris, and adjacent structures. These structures are visible on inspection. (See Structures of the female reproductive system, pages 36 and 37.)
|
Mons pubis
The mons pubis is a rounded cushion of fatty and connective tissue covered by skin and coarse, curly hair in a triangular pattern over the symphysis pubis (the joint formed by the union of the pubic bones anteriorly).
Labia majora
The labia majora are two raised folds of adipose and connective tissue that border the vulva on either side, extending from the mons pubis to the perineum. After onset of the first menses (called menarche), the outer surface of the labia is covered with pubic hair. The inner surface is pink and moist.
Labia minora
The labia minora are two moist folds of mucosal tissue, dark pink to red in color, that lie within and alongside the labia majora. Each upper section divides into an upper and
lower lamella. The two upper lamellae join to form the prepuce, a hoodlike covering over the clitoris. The two lower lamellae form the frenulum, the posterior portion of the clitoris.
lower lamella. The two upper lamellae join to form the prepuce, a hoodlike covering over the clitoris. The two lower lamellae form the frenulum, the posterior portion of the clitoris.
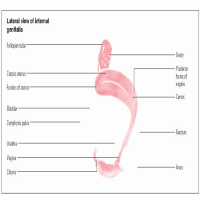
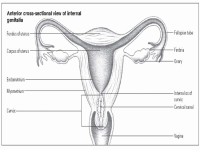
Structures of the female reproductive system
The female reproductive system consists of external and internal genitalia. These structures include the vagina, cervix, uterus, fallopian tubes, ovaries, and other structures. Reproductive, urinary, and gastrointestinal (GI) structures are housed in the female pelvis. These include the bladder, anus, and rectum.
|
|
|
The lower labial sections taper down and back from the clitoris to the perineum, where they join to form the fourchette, a thin tissue fold along the anterior edge of the perineum.
Minor in name only
The labia minora contain sebaceous glands, which secrete a lubricant that also acts as a bactericide. Like the labia majora, they’re rich in blood vessels and nerve endings, making them highly responsive to stimulation. They swell in response to sexual stimulation, a reaction that triggers other changes that prepare the genitalia for coitus.
Clitoris
The clitoris is the small, protuberant organ just beneath the arch of the mons pubis. It contains erectile tissue, venous cavernous spaces, and specialized sensory corpuscles, which are stimulated during sexual activity.
Adjacent structures
The vestibule is an oval area bounded anteriorly by the clitoris, laterally by the labia minora, and posteriorly by the fourchette.
Featuring glands
The mucus-producing Skene glands are found on both sides of the urethral opening. Openings of the two mucus-producing Bartholin glands are located laterally and posteriorly on either side of the inner vaginal orifice.
The urethral meatus is the slitlike opening below the clitoris through which urine leaves the body. In the center of the vestibule is the vaginal orifice. It may be completely or partially covered by the hymen, a tissue membrane.
Not too simple
Located between the lower vagina and the anal canal, the perineum is a complex structure of muscles, blood vessels, fasciae, nerves, and lymphatics.
Internal genitalia
The female internal genitalia include the vagina, cervix, uterus, fallopian tubes, ovaries, and mammary glands. The main function of these specialized organs is reproduction.
Vagina
The vagina, a highly elastic muscular tube, is located between the urethra and the rectum.
Three layers …
The vaginal wall has three tissue layers: epithelial tissue, loose connective tissue, and muscle tissue. The uterine cervix connects the uterus to the vaginal vault. Four fornices (the anterior fornix, posterior fornix, and left lateral and right lateral fornix), recesses in the vaginal wall, surround the cervix.
… three functions
The vagina has three main functions:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access