Chronic Bronchitis and Emphysema
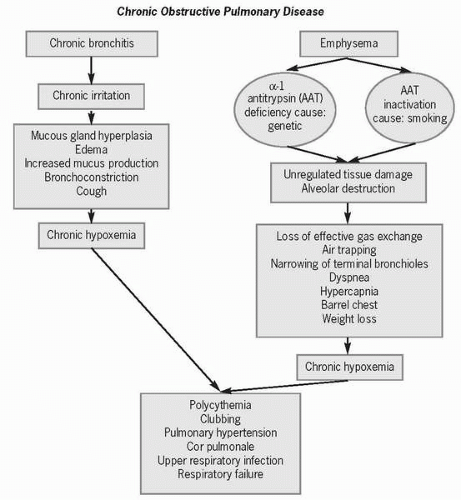
Chronic obstructive pulmonary disease (COPD) occurs when there is chronic, often progressive, airflow limitation related to chronic bronchitis or emphysema. It has been estimated that 28 million people have COPD, although only 50% have been diagnosed. The death rate from COPD is increasing, with elderly men the most affected.
Approximately one in four adults in the United States has chronic bronchitis, which is defined as inflammation of the bronchi, a productive cough, and increased mucus production for at least 3 months of the year for 2 consecutive years. Current or former smokers are at greatest risk for developing this disease, as are people exposed to inhaled irritants such as second-hand cigarette smoke and air pollution.
 Chronic obstructive pulmonary disease (COPD) occurs when there is chronic, often progressive, airflow limitation related to chronic bronchitis or emphysema. It has been estimated that 28 million people have COPD, although only 50% have been diagnosed.
Chronic obstructive pulmonary disease (COPD) occurs when there is chronic, often progressive, airflow limitation related to chronic bronchitis or emphysema. It has been estimated that 28 million people have COPD, although only 50% have been diagnosed. Current or former smokers are at greatest risk for developing chronic bronchitis.
Current or former smokers are at greatest risk for developing chronic bronchitis.Emphysema, which affects 2.5 million Americans, is an anatomical term that denotes loss of lung elasticity as a result of the breakdown of connective tissue support of the lower airways, abnormal dilatation of air spaces distal to the terminal bronchioles, and abnormal enlargement and eventual destruction of the alveoli. Risk factors for developing emphysema include chronic bronchitis, smoking, and air pollution.
Chronic Bronchitis
As a defense against airborne irritants, the upper and mid-airways set up an inflammatory response that result in mucus gland hyperplasia, edema, increased thick mucus production, bronchoconstriction, and cough. Airway resistance affects both inspiration and expiration, resulting in hypoventilation, hypoxemia, cyanosis, hypercapnia, increased red blood cell production (i.e., polycythemia), clubbing of the fingers, and eventually, shortness of breath even at rest.
 As a defense against airborne irritants, the upper and mid-airways set up an inflammatory response.
As a defense against airborne irritants, the upper and mid-airways set up an inflammatory response. Chronic hypoxemia causes reflexive pulmonary vascular narrowing called pulmonary hypertension.
Chronic hypoxemia causes reflexive pulmonary vascular narrowing called pulmonary hypertension.Chronic hypoxemia causes reflexive pulmonary vascular narrowing called pulmonary hypertension. As the right ventricle hypertrophies in an attempt to overcome increased pulmonary
artery resistance, cor pulmonale (i.e., right-sided heart failure) develops.
artery resistance, cor pulmonale (i.e., right-sided heart failure) develops.
 As the right ventricle hypertrophies in an attempt to overcome increased pulmonary artery resistance, cor pulmonale (i.e., right-sided heart failure) develops.
As the right ventricle hypertrophies in an attempt to overcome increased pulmonary artery resistance, cor pulmonale (i.e., right-sided heart failure) develops.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access