Cardiovascular Emergencies
1. Which drug shouldn’t be given by way of an endotracheal (ET) tube?
[ ] A. Atropine
[ ] B. Sodium bicarbonate
[ ] C. Epinephrine
[ ] D. Lidocaine (Xylocaine)
View Answer
Correct answer—B. Rationales: Sodium bicarbonate shouldn’t be given by way of an ET tube because of its alkalinity and because the large amounts required shouldn’t be administered by this route. Atropine, epinephrine, and lidocaine are absorbed rapidly by the lungs and may be given safely by way of an ET tube.
Nursing process step: Intervention
2. A client has the following symptoms: dyspnea, dependent edema, hepatomegaly, crackles, and distended jugular veins. The nurse should suspect which condition?
[ ] A. Pulmonary embolism
[ ] B. Heart failure
[ ] C. Cardiac tamponade
[ ] D. Tension pneumothorax
View Answer
Correct answer—B. Rationales: A client with heart failure has reduced cardiac output because of the heart’s decreased pumping ability. Therefore, fluid builds up and causes dyspnea, edema, hepatomegaly, crackles, and distended jugular veins. A client with pulmonary embolism has acute shortness of breath, pleuritic chest pain, hemoptysis, and fever. A client with cardiac tamponade has muffled heart sounds, hypotension, and elevated venous pressure. A client with tension pneumothorax has a deviated trachea and no breath sounds on the affected side as well as dyspnea and distended jugular veins.
Nursing process step: Assessment
3. A client arrives in the emergency department complaining of nausea, diaphoresis, shortness of breath, and squeezing substernal pain that radiates to the left shoulder and teeth. The nurse should perform which intervention?
[ ] A. Complete registration, order an electrocardiogram, establish I.V. access, and record vital signs.
[ ] B. Alert the catheter laboratory team, administer oxygen, apply a cardiac monitor, and notify the physician.
[ ] C. Take the client to the examination room, establish I.V. access, give sublingual nitroglycerin, and alert the catheter laboratory team.
[ ] D. Administer oxygen, apply a cardiac monitor, record the client’s vital signs, and give sublingual nitroglycerin.
View Answer
Correct answer—D. Rationales: The client’s pain is caused by myocardial ischemia. Oxygen increases the myocardial oxygen supply. Cardiac monitoring reveals life-threatening arrhythmias. The nurse should ensure that the client isn’t hypotensive before giving sublingual nitroglycerin for chest pain. Registration may be delayed until the client is stabilized. Alerting the catheter laboratory team before completing an initial assessment is premature.
Nursing process step: Intervention
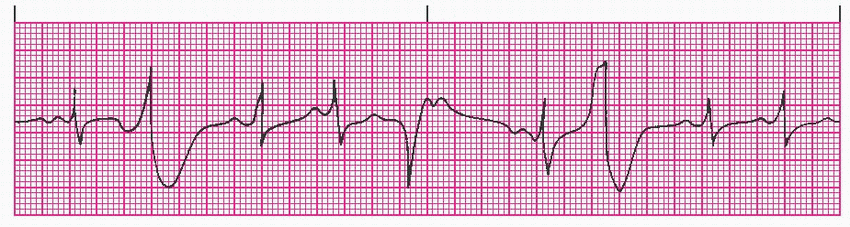
4. The cardiac monitor reveals the following rhythm on a client who’s complaining of substernal chest pains.
|
After administering oxygen by nasal cannula, what medication would be the initial treatment for this arrhythmia?
[ ] A. Magnesium sulfate
[ ] B. Amiodarone
[ ] C. Lidocaine (Xylocaine)
[ ] D. Atropine
View Answer
Correct answer—C. Rationales: The client is experiencing premature ventricular contractions (PVCs). Lidocaine is the drug of choice for PVCs associated with chest pain and a normal heart rate. Magnesium sulfate is used in torsades de pointes. Amiodarone is used only for life-threatening ventricular arrhythmias. Atropine is used to increase heart rate, which is not necessary in this situation.
Nursing process step: Intervention
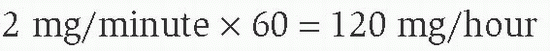
5. The nurse is asked to begin a lidocaine infusion. The premixed bag contains 2 g of lidocaine in 500 mL of dextrose 5% in water. What’s the drip rate for 2 mg/minute to be delivered by infusion pump?
[ ] A. 15 mL/hour
[ ] B. 30 mL/hour
[ ] C. 45 mL/hour
[ ] D. 60 mL/hour
View Answer
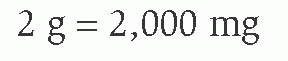
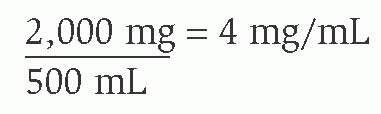
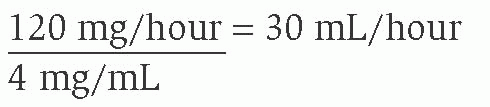
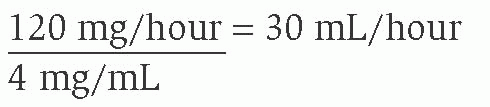
Correct answer—B. Rationales: First determine the concentration:
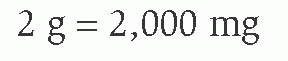
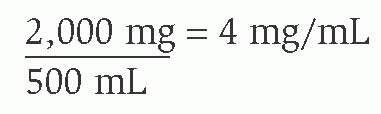
Then determine the drip rate:
Nursing process step: Intervention
6. Which of the following is an absolute contraindication for thrombolytic therapy?
[ ] A. Active bleeding
[ ] B. Current anticoagulant therapy
[ ] C. Over age 75
[ ] D. Severe hepatic disease
View Answer
Correct answer—A. Rationales: Active bleeding is an absolute contraindication for thrombolytic therapy. The other options are considered relative risks and should be evaluated before administering thrombolytics.
Nursing process step: Assessment
7. Which of the following are complications of thrombolytic (reperfusion) therapy?
[ ] A. Puncture site oozing and GI bleeding
[ ] B. Tachycardia
[ ] C. Chest pain
[ ] D. Headache
View Answer
Correct answer—A. Rationales: Bleeding is a complication of thrombolytic therapy. Bradycardia—not tachycardia—is a common reperfusion arrhythmia (others are accelerated idioventricular and ventricular ectopy). The client should also have less chest pain. Headache isn’t associated with thrombolytic therapy.
Nursing process step: Assessment
8. Diuretic therapy is deemed effective in a client with heart failure if:
[ ] A. dyspnea decreases and jugular vein distention (JVD) increases.
[ ] B. JVD decreases and urine output increases.
[ ] C. dyspnea decreases, urine output increases, and JVD decreases.
[ ] D. dyspnea decreases and JVD decreases.
View Answer
Correct answer—C. Rationales: Diuretics decrease preload by eliminating sodium and water from the body and decrease dyspnea, increase urine output, and decrease JVD.
Nursing process step: Evaluation
9. A client with acute heart failure exhibits these hemodynamic parameters: central venous pressure, 15 mm Hg; blood pressure, 90/50 mm Hg; pulse, 132 beats/minute; and respirations, 36 breaths/minute. What are the therapy goals for this client?
[ ] A. To decrease myocardial workload, decrease volume, and increase myocardial contractility
[ ] B. To decrease volume, decrease cardiac output, and increase myocardial contractility
[ ] C. To increase volume, decrease cardiac output, and increase myocardial contractility
[ ] D. To decrease myocardial workload, increase volume, and increase myocardial contractility
View Answer
Correct answer—A. Rationales: Therapy goals for a client with acute heart failure are to reduce myocardial workload in order to increase cardiac output; decrease volume, which causes dyspnea and edema; and increase myocardial contractility to increase cardiac output. Heart failure is a low cardiac output state.
Nursing process step: Evaluation
10. A 34-year-old client is brought to the emergency department with a stab wound to the right lower chest. His vital signs are as follows: blood pressure, 80/50 mm Hg; pulse, 130 beats/minute; and respirations, 24 breaths/minute. Breath sounds are present bilaterally, and heart sounds are muffled. Based on these assessment findings, what should the nurse anticipate happening next?
[ ] A. Computed tomography (CT) of the chest
[ ] B. Pericardiocentesis
[ ] C. Central venous catheter insertion
[ ] D. Chest tube insertion
View Answer
Correct answer—B. Rationales: Based on the assessment findings of both hypotension and muffled heart sounds, the client is experiencing cardiac tamponade. Immediate intervention by way of pericardiocentesis is necessary to correct the problem in order to prevent the client from experiencing cardiac arrest. CT of the chest will confirm fluid accumulation around the pericardium but will delay treatment. Insertion of the central venous catheter may be needed for fluid replacement in the absence of I.V. access. Insertion of a chest tube isn’t necessary at this time because the client has equal breath sounds bilaterally.
Nursing process step: Analysis
11. A 75-year-old male is brought to the emergency department. He’s complaining of chest pain, headaches, and blurred vision. He states he has a history of hypertension but hasn’t been taking his medication because he ran out. Vital signs are as follows: blood pressure, 210/130 mm Hg; pulse, 110 beats/minute, and regular and respiratory rate of 18 breaths/minute. Breath sounds are clear bilaterally, and pulse oximetry is 98% on room air. Based on the above assessment findings, what might this client be experiencing?
[ ] A. Acute myocardial infarction (MI)
[ ] B. Heart failure
[ ] C. Hypertensive crisis
[ ] D. Pericarditis
View Answer
Correct answer—C. Rationales: The client presents with a blood pressure of 210/130 mm Hg, blurred vision, headaches, and chest pain, which are all consistent findings of a client experiencing a hypertensive crisis. The findings listed here aren’t consistent with acute MI, heart failure, or pericarditis.
Nursing process step: Analysis
12. In order to control a hypertensive crisis and prevent further damage, the physician orders labetalol I.V. push. To ensure safe medication administration, what should the nurse keep in mind?
[ ] A. Dilute the medication and hang as a piggyback.
[ ] B. Administer the medication over 10 seconds.
[ ] C. Place the client on a cardiac monitor and noninvasive blood pressure monitoring.
[ ] D. Divide into 4 equal doses for administration.
View Answer
Correct answer—C. Rationales: Labetalol administration can cause hypotension, bradycardia, and heart blocks, so monitoring of both the blood pressure and the heart rate and rhythm is essential for safe administration. It isn’t necessary to dilute the medication and hang as a piggyback. Labetalol can be administered I.V. push over 2 minutes—not 10 seconds. Labetalol doesn’t need to be divided into 4 equal doses for administration.
Nursing process step: Intervention
13. The emergency department nurse should prepare a client with a ruptured aorta for:
[ ] A. emergency surgery.
[ ] B. chest tube insertion.
[ ] C. chest computed tomography (CT) scan.
[ ] D. immediate intubation.
View Answer
Correct answer—A. Rationales: A client with a ruptured aorta requires immediate surgery. Chest tubes shouldn’t be inserted. Diagnosis can be made with chest X-ray. A CT scan would delay definitive treatment. Intubation is done at the time of surgery, unless otherwise indicated.
Nursing process step: Intervention
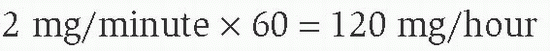
14. A client with hypotension and dyspnea has the following rhythm:
|
The emergency nurse should immediately do which of the following?
[ ] A. Administer lidocaine (Xylocaine) 1 mg/kg I.V. push.
[ ] B. Prepare for external pacing.
[ ] C. Administer atropine 0.5 mg I.V. push.
[ ] D. Begin a dopamine infusion at 5 g/kg per minute.
View Answer
Correct answer—C. Rationales: The client’s ECG strip shows bradycardia, and atropine is the drug of choice for treating symptomatic bradycardia. The 2010 American Heart Association guidelines recommend repeating the 0.5-mg dose at 3- to 5-minute intervals until 3 mg has been given. Pacing may be indicated if atropine is ineffective. Dopamine isn’t a first-line drug for treating bradycardia. However, it’s used to treat hypotension. In this case, bradycardia is the cause of hypotension and should be addressed first. Lidocaine shouldn’t be given for bradycardia because it may suppress the escape rhythm and lead to further hypotension and, possibly, asystole.
Nursing process step: Intervention
15. The nurse has delivered synchronized cardioversion to a symptomatic client with supraventricular tachycardia. The client then develops pulseless ventricular tachycardia. What should the nurse do immediately?
[ ] A. Deliver a precordial thump.
[ ] B. Administer lidocaine (Xylocaine) 1 mg/kg I.V. push.
[ ] C. Defibrillate at 200 joules.
[ ] D. Administer adenosine (Adenocard) 6 mg I.V. push.
View Answer
Correct answer—C. Rationales: Immediately defibrillate at 200 joules according to advanced cardiac life support protocol. A precordial thump isn’t part of the 2010 American Heart Association guidelines. Lidocaine can be administered as an alternative to amiodarone for persistent pulseless ventricular tachycardia if defibrillation and epinephrine are ineffective. Adenosine isn’t effective for ventricular tachycardias.
Nursing process step: Intervention
16. An 80-year-old client has received a lidocaine bolus and infusion after suffering nonsustained ventricular tachycardia. For which symptom of lidocaine toxicity should the nurse monitor?
[ ] A. Hypertension
[ ] B. Tachycardia
[ ] C. Increased intracranial pressure
[ ] D. Seizures
View Answer
Correct answer—D. Rationales: Seizures are a symptom of lidocaine toxicity. Hypertension, tachycardia, and increased intracranial pressure aren’t commonly associated with lidocaine toxicity.
Nursing process step: Evaluation
17. Which of the following best demonstrates the effectiveness of thrombolytic therapy?
[ ] A. Greater than 2-mm elevation in the ST segment
[ ] B. Oozing from I.V. sites
[ ] C. Relief of chest pain
[ ] D. Absence of arrhythmias
View Answer
Correct answer—C. Rationales: Thrombolytic therapy effectiveness is measured by the relief of chest pain, presence of reperfusion arrhythmias, and normalization of the ST segment. Oozing of blood from I.V. sites may occur because thrombolytic therapy may increase bleeding time, but bleeding doesn’t demonstrate its effectiveness.
Nursing process step: Assessment
18. Which intervention is inappropriate for a client with acute arterial occlusion?
[ ] A. Maintain the affected extremity in a dependent position.
[ ] B. Apply a heating pad to the affected extremity.
[ ] C. Use a Doppler ultrasound device to auscultate pulses.
[ ] D. Prepare the client for possible surgery.
View Answer
Correct answer—B. Rationales: Increased temperature increases oxygen demands on the extremity. Maintaining the extremity in a dependent position promotes blood flow. Using Doppler ultrasound aids in assessing for worsening of the occlusion. The client may need surgery.
Nursing process step: Intervention
19. A client who has been kicked in the chest by a bull arrives in the emergency department. Vital signs are blood pressure, 80/50 mm Hg; pulse, 144 beats/minute; respirations, 36 breaths/minute; and temperature, 98.5° F (36.9° C). Heart sounds are muffled and facial cyanosis is present. A bolus of 1,000 mL of fluid is infused. Blood pressure remains 82/50 mm Hg and pulse increases to 150 beats/minute. The client is most likely to have:
[ ] A. myocardial contusion.
[ ] B. tension pneumothorax.
[ ] C. cardiac tamponade.
[ ] D. aortic injury.
View Answer
Correct answer—C. Rationales: Muffled heart sounds are associated with cardiac tamponade. A volume-depleted client with cardiac tamponade may not respond to volume infusion. Myocardial contusion presents with chest pain and electrocardiogram changes. Tension pneumothorax presents with acute increases in respiratory rate and heart rate, chest pain, tracheal deviation to the unaffected side, and an absence of breath sounds on the affected side. Aortic injury presents with a widened mediastinum by chest X-ray, hypotension, respiratory distress, and chest pain.
Nursing process step: Assessment
20. The aorta is most commonly injured during which type of trauma?
[ ] A. Deceleration trauma that causes shearing
[ ] B. Penetrating trauma
[ ] C. Blunt chest trauma
[ ] D. Chest injuries that cause rib fractures
View Answer
Correct answer—A. Rationales: Deceleration may cause laceration to the aorta by shearing forces. The other options may cause aortic injuries but aren’t the primary mechanisms of injury.
Nursing process step: Assessment
21. A client is undergoing pericardiocentesis. The rhythm previously showed sinus tachycardia.
Premature ventricular contractions (PVCs) are now noted on the monitor. This condition indicates which of the following?
[ ] A. It’s time for the physician to begin aspirating the syringe.
[ ] B. The pericardial sac has been entered, and it’s time to attach a clamp to the needle at the skin level to prevent further insertion.
[ ] C. The needle has entered the heart.
[ ] D. The needle is touching the myocardium.
View Answer
Correct answer—D. Rationales: If the needle touches the myocardium, PVCs or ST-segment elevation may be observed. The needle hasn’t necessarily entered the heart. At this time, the needle should be withdrawn slightly. The physician should aspirate the syringe while advancing the needle and should stop as soon as blood is obtained.
Nursing process step: Intervention
22. Cardiac tamponade may result from which condition?
[ ] A. Myasthenia gravis
[ ] B. Endocarditis
[ ] C. Systemic lupus erythematosus
[ ] D. Guillain-Barré syndrome
View Answer
Correct answer—C. Rationales: Systemic lupus erythematosus as well as chest trauma and pericarditis may cause an accumulation of fluid in the pericardial sac, leading to cardiac tamponade. The other options don’t result in cardiac tamponade.
Nursing process step: Evaluation
23. A client with a ruptured descending aorta may exhibit which of the following?
[ ] A. Greater pulse amplitude in the arms than in the legs
[ ] B. Greater pulse amplitude in the legs than in the arms
[ ] C. Blood pressure differences in right and left arms
[ ] D. Distended jugular veins and muffled heart sounds
View Answer
Correct answer—A. Rationales: A client with a ruptured descending aorta may have a greater pulse amplitude in the arms than in the legs because of decreased perfusion to the legs. Blood pressure differences in arms are indicative of ruptured subclavian arteries. Distended jugular veins and muffled heart sounds aren’t likely to be present in this client.
Nursing process step: Assessment
24. A client with electrocardiogram (ECG) changes in leads V1, V2, and V3 may be suffering from which injury?
[ ] A. Inferior wall injury
[ ] B. Anterior wall injury
[ ] C. Lateral wall injury
[ ] D. Posterior wall injury
View Answer
Correct answer—B. Rationales: Anterior wall injury is associated with ECG changes in leads V1, V2, and V3. Inferior wall injury is associated with ECG changes in leads II, III, and aVF. Lateral wall injury is associated with ECG changes in leads I, aVL, V5, and V6. Posterior wall injury is associated with ECG changes in leads V1 and V2.
Nursing process step: Assessment
25. A client with a history of hypertension and coronary artery disease (CAD) presents with substernal chest pain and shortness of breath. The pain is unrelieved with multiple doses of nitroglycerin and the administration of oxygen, but it responds to morphine. This may indicate that the pain is caused by:
[ ] A. angina pectoris because this type of pain is usually unresponsive to nitroglycerin and oxygen administration.
[ ] B. acute myocardial infarction (MI) because the pain of acute MI isn’t usually relieved by nitroglycerin and oxygen administration.
[ ] C. heart failure because this may cause chest pain that’s unrelieved by nitroglycerin and oxygen administration.
[ ] D. pericarditis because this disorder is commonly seen in a hypertensive client with CAD and won’t respond to nitroglycerin or oxygen administration.
View Answer
Correct answer—B. Rationales: The pain of acute MI won’t be relieved by the administration of nitroglycerin. This differentiates it from anginal pain, which should respond to nitroglycerin administration and oxygen. Heart failure isn’t commonly associated with substernal chest pain, and pericarditis isn’t common in a hypertensive client with CAD.
Nursing process step: Assessment
26. A client in ventricular fibrillation hasn’t responded to standard treatment—defibrillation, epinephrine, and lidocaine (Xylocaine). Which of the following is a potentially reversible cause of ventricular fibrillation?
[ ] A. Hypothermia
[ ] B. Hypervolemia
[ ] C. Hyperthermia
[ ] D. Digoxin toxicity
View Answer
Correct answer—A. Rationales: Hypothermia, hypovolemia, and electrolyte imbalances can potentially cause ventricular fibrillation and may need to be treated before standard measures are effective. Digoxin toxicity can cause atrial tachycardia—not ventricular fibrillation.
Nursing process step: Evaluation
27. What’s the maximum number of times a client can be defibrillated safely?
[ ] A. 10
[ ] B. 15
[ ] C. 18
[ ] D. There’s no limit
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access