Evidence Base
Evidence Base
One million burn injuries are reported each year, resulting in 3,500 deaths as a result of fire and burns in the United States, with a survival rate of 96%. This is a significant decline from 2 million burn injuries in the early 1990s.
Seven hundred thousand patients visit the emergency department every year for a burn injury and 45,000 patients require admission and about one half of those patients are treated at a specialized burn center.
The average burn size is 14% total body surface area (TBSA).
Males (70%) are more commonly injured by burns than are females.
Flame injury (44%) is the leading cause of accidents for adults and scalding (33%) is the leading cause of accidents for children. Fires in the home, combined with smoke inhalation, account for most burn-related deaths.
 Evidence Base
Evidence Base
A burn injury usually results from energy transfer from a heat source to the body. The type of burn injury may be flame/flash, contact, scald (water, grease), chemical, electrical, inhalation, or any thermal source. Many factors alter the response of body tissues to these sources of heat.
Local tissue conductivity—bone is most resistant to the heat source accumulation. Lesser resistance is seen in nerves, blood vessels, and muscle tissue.
Adequacy of peripheral circulation.
Skin thickness, insulating material of clothing, or dampness of the skin.
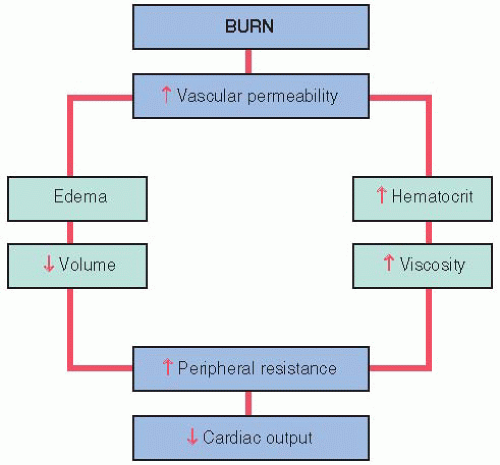
Physiologic reaction to a burn is a unique combination of distributive and hypovolemic shock. The release of mediators such as tumor necrosis factor-α produce a profound effect on the circulatory system. In burns greater than 20% TBSA, there is an intravascular depletion, low pulmonary artery occlusion pressures, elevated systemic vascular resistance, and depressed cardiac output.
Systemic microcirculation loses its vessel wall integrity and proteins are lost into the interstitium.
Protein loss causes intravascular colloid osmotic pressure to drop and allows fluid to leak from the vessels.
There is an increase of fluid leaking into the interstitium, caused by decreased interstitial pressure and increased capillary permeability to protein.
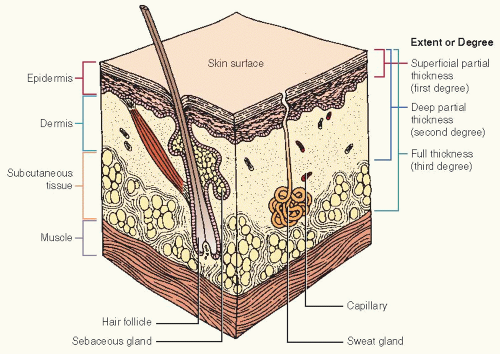
Figure 34-1. Cross-section of skin depicting blood supply, depth of burn, and relative thickness of skin grafts. (The Burn Patient, Ethicon.)
Over 24 hours, there is a loss of intravascular fluid, electrolytes, and proteins into the interstitium.
The resultant changes are reflected in massive edema formation, loss of circulating plasma volume, hemoconcentration, decreased urine output, and depressed cardiac function.
Burns may be partial (second-degree) or full (third-degree) thickness (see Figure 34-1).
Superficial partial-thickness burns are commonly termed first-degree burns. Only the epidermis is involved. Local redness, blanching occurs similar to a sunburn. Healing time is 5 to 7 days.
Deep partial-thickness burn injuries, commonly known as second-degree burns, involve the epidermis and upper portions of the dermis. Sweat glands, hair follicles, and nerves remain intact. The wound is moist and very painful. Some of the dermal appendages remain, from which the wound can spontaneously reepithelialize and heal on its own. A deep partial-thickness burn injury can convert to a full-thickness burn injury if patient is underresuscitated or develops an infection. Healing time is 5 to 35 days.
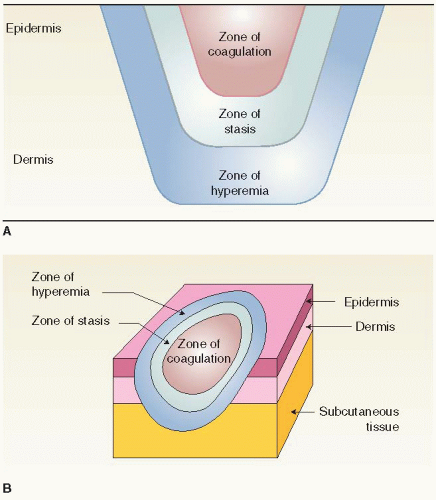
Full-thickness injuries, commonly known as third-degree burns, involve all layers of the skin and sometimes underlying tissues are destroyed. The burn wound is dry, white, brown, or leathery in appearance. Patients typically do not have pain with full-thickness injuries due to the destruction of the nerve endings. At the core is the burn injury. There is then a zone of coagulation surrounded by a zone of stasis, surrounded by hyperemia (erythema) very similar to a bull’s-eye pattern, the burn being in the center (see Figure 34-2). Grafting is usually required to close the wound.
Burn depth is directly related to the temperature of the burning agent and the duration of contact with body tissue.
Below 112° F (44.4° C), no local damage occurs unless exposure is for a protracted period.
At 120° F (48.9° C), it takes 5 minutes’ exposure to create a full-thickness burn.
At 125° F (51.7° C) the time requirement is 2 minutes, and at 140° F (60° C) only 6 seconds is required.
At 159° F (70.6° C) it takes 1 second to create a full-thickness burn in a healthy adult—less time or temperature in children or older adults.
 Evidence Base
Evidence Base
The burn injury results in a release of mediators and an activation of neutrophils and a release of free radicals. In the lungs, free radicals are toxic and it is this injury pattern that is more significant than the thermal injury itself. Inhalation injuries combined with a large burn injury accounts for most mortality from a burn injury.
Most inhalation injuries that result in death are a result of carbon monoxide. It is a colorless, odorless, tasteless, nonirritating gas produced from incomplete combustion of carboncontaining materials.
Carbon monoxide’s affinity for hemoglobin is 200 times greater than for oxygen.
Toxicity depends on concentration of carbon monoxide in inspired air and the length of time of exposure.
Although oxygen content of the blood is diminished, the amount of dissolved oxygen in the plasma (PaO2) is unaffected by carbon monoxide poisoning; therefore, the arterial blood gas will appear normal.
Pulse oximetry only detects saturated hemoglobin and does not measure carbon monoxide; therefore, the pulse oximetry will appear normal.
A serum carboxyhemoglobin level must be measured in any patient with possible exposure to carbon monoxide in a fire.
A carboxyhemoglobin level of less than 10% is not a cause for alarm. Normal carboxyhemoglobin in nonsmokers is less than 5% and smokers can have carboxyhemoglobin levels as high as 10%.
From 10% to 20%, severe headache, flushing, and dilation of skin vessels occur.
Levels of 30% to 50% can produce disorientation, nausea, irritability, dizziness, vomiting, prostration, tachypnea, and tachycardia.
Levels above 50% result in coma, seizures, convulsions, and Cheyne-Stokes respirations, and death is possible.
Sulfur dioxide and nitrous oxide are toxic agents inhaled in soot. In the presence of water, they form corrosive acids and alkalis that are extremely toxic.
Toxic fumes from burning plastic are more dangerous than smoke.
Noxious gases include hydrogen cyanide, hydrochloric acid, sulfuric acid, halogens, and perhaps phosgene.
Restrictive pulmonary complications can occur because of the tourniquet effect of edema seen with circumferential chest burns. Lung compliance and alveolar gas exchange can also be decreased because of acute respiratory distress syndrome (ARDS).
 Evidence Base
Evidence Base
In addition to changes in the local burned area, there are alterations and disruptions in the vascular and other systems of the body.
The water-vapor barrier for the body is the outermost layer of the epidermis. When it is rendered nonfunctioning, severe systemic reactions from fluid losses can occur.
Fluid volume deficit is directly proportional to the extent and depth of burn injury.
Capillary permeability increases, permitting fluid and protein to move from vascular to interstitial spaces (edema results) for the first 24 to 36 hours, peaking at 12 hours postburn. Protein-rich fluid is lost in blebs of the burned tissues as well as by weeping of second-degree wounds and surface of full-thickness wounds. With reduced vascular volume, the patient will go into shock if untreated.
Capillary permeability starts to change in about 48 hours, but protein lost in interstitial spaces may remain there for 5 days to 2 weeks before returning to the vascular system.
When fluid mobilizes (moves from interstitial spaces back to vascular compartment), patients with good cardiac and renal function will diurese.
Patients with impaired cardiac or renal function are in danger of fluid overload and pulmonary edema at this time.
Red blood cell (RBC) mass is also diminished because of thrombosis, sludging, and RBC death from thermal injury; as fluid escapes from capillary walls, however, blood concentrates and the hematocrit rises, causing sluggish flow (see Figure 34-3).
Capillary stasis may cause ischemia and even necrosis.
The body attempts to compensate for losses of plasma volume.
Constriction of vessels.
Withdrawal of fluid from undamaged extracellular space.
Patient thirst.
Decreased circulating blood and plasma volume results in decreased cardiac output initially and increased pulse rate as a result of hypovolemia.
Afterload is increased due to a marked increase in systemic vascular resistance resulting from vasoactive mediators such as catecholamines.
A decrease in cardiac contractility is a predominant feature of full-thickness injuries covering more than 40% TBSA.
This results in inadequate tissue perfusion, which may in turn cause metabolic acidosis, renal failure, and irreversible burn shock.
Electrolyte imbalance may also occur.
Hyponatremia usually occurs during the 3rd to 10th day due to fluid shift.
The burn injury also causes hyperkalemia initially due to cell destruction, followed by hypokalemia as fluid shifts occur if potassium is not replaced.
The initial metabolic response is thought to be activated by proinflammatory cytokines. The release of catecholamines, cortisol, glucagon, renin-angiotensive, antidiuretic hormone, and aldosterone is also increased. The major fuel source is stored glycogen. Major hypermetabolism and catabolism occur immediately postburn. The degree of the response is directly proportionate to the size of the burn injury.
Tachycardia, ranging from 100 to 120 beats per minute, is common and results from persistent elevation of catecholamine levels.
“Burn fever” (usually seen during the first week) is common and is dependent on depth of burn and percentage of TBSA involved. An increase of 1° F to 2° F makes it difficult to assess for infection.
Total body glucose stores are limited and stored liver and muscle glycogen is exhausted within the first few days postburn, hepatic glucose synthesis (gluconeogenesis) increases and patients with glucose intolerance (obese patients and older adults) usually develop hyperglycemia.
Increased catabolism leads to increased urea production, especially in nutritionally depleted patients.
Body levels of protein begin to decrease as high levels of cortisol, inflammatory cytokines continue to circulate. Skeletal and visceral protein are mobilized to meet increased nutritional demands. Ten to 15% of body protein stores can be lost within 10 days without proper nutritional supplementation. This can lead to muscular weakness, decreased wound healing, and further weakening of the immune system.
With adequate fluid resuscitations, the patient’s weight will increase during the first few days. Fluid mobilization will result in weight loss, as will the catabolic response. Nutritional support in the form of enteral or total parenteral nutrition may be necessary. Weight loss from fluid mobilization usually starts within 3 to 4 days postresuscitation.
Despite all nutritional support, it is almost impossible to counteract a negative nitrogen balance; the sooner a burn wound is closed, the more rapidly a positive nitrogen balance is reached.
The resting metabolic expenditure increases linearly with amount of TBSA; a burn of 40% to 50% TBSA has a metabolic rate almost twice normal.
The adult burn patient may require 3,000 to 5,000 calories or more per day.
A burn of less than 10% usually requires minimal supplementation.
A high-protein, high-calorie diet is necessary for a 10% to 20% burn.
Between 20% and 30%, enteral feedings are generally necessary.
TBSA burns of 30% to 40% may require total parenteral nutrition. However, the current trend is to meet nutritional needs enterally, if possible.
Glomerular filtration may be decreased in extensive injury.
Without resuscitation or with delay, decreased renal blood flow may lead to high output or oliguric renal failure and decreased creatinine clearance.
Hemoglobin and myoglobin, present in the urine of patients with deep muscle damage commonly associated with electrical injury, may cause acute tubular necrosis and call for a greater amount of initial fluid therapy and osmotic diuresis.
Hyperventilation and increased oxygen consumption are associated with major burns.
The majority of deaths from fire are due to smoke inhalation.
Overzealous fluid resuscitation and the effects of burn shock on cell membrane potential may cause pulmonary edema, contributing to decreased alveolar exchange. Therefore, with an inhalation injury, it may be necessary to keep the patient slightly less hydrated.
Initial respiratory alkalosis resulting from hyperventilation may change to respiratory acidosis associated with pulmonary insufficiency as a result of major burn trauma.
Thrombocytopenia, abnormal platelet function, depressed fibrinogen levels, inhibition of fibrinolysis, and a deficit in several plasma clotting factors occur postburn.
Anemia results from the direct effect of destruction of RBCs due to burn injury, reduced life span of surviving RBCs, overt or (more commonly) occult blood loss from duodenal or gastric ulcers, and blood loss during diagnostic and therapeutic procedures.
The loss of the skin barrier and presence of eschar favor bacterial growth. Methicillin-resistant Staphylococcus aureus (MRSA) is now being seen in the immunocompromised burn patient.
Polymorphonuclear chemotactic activity is suppressed, which results in decreased oxygen consumption and impaired bactericidal activity.
Abnormal inflammatory response after burn injury causes a decreased delivery of antibiotics, white blood cells, and oxygen to the injured area.
Hypoxia, acidosis, and thrombosis of vessels in the wound area impair host resistance to pathogenic bacteria.
Serum IgA, IgM, and IgG are depressed, reflecting depressed B cell function.
Depressed cellular immunity is reflected by lymphocytopenia, delayed skin sensitivity, decreased allograft rejection potential, depletion of thymus-dependent lymphoid tissue, and increased susceptibility to fungi, viruses, and Gram-negative organisms.
Burn wound sepsis.
After colonization of the burn wound surface by bacteria, subeschar, and intrafollicular colonization develop. Intraeschar and subeschar colonization may progress to invasion of subadjacent, nonburned, previously viable tissue.
A bacterial count of 105 per gram of tissue as determined by burn wound biopsy (quantitative culture) indicates burn wound sepsis. Usually, only a swab culture is done of the wound surface.
The wound is fully colonized in 3 to 5 days.
Seeding of bacteria from the wound may give rise to systemic septicemia.
As a result of sympathetic nervous system response to trauma, peristalsis decreases and gastric distention, nausea, vomiting, and paralytic ileus may occur.
Ischemia of the gastric mucosa and other etiologic factors put the burn patient at risk for duodenal and gastric ulcers, manifested by occult bleeding and, in some cases, life-threatening hemorrhage.
Depth—first-, second- (partial-thickness), third-degree (fullthickness).
Extent—percentage of TBSA.
Age—the very young and very old have a poor prognosis; the prognosis alters for adults after age 45.
Area of the body burned—face, hands, feet, perineum, and circumferential burns require special care.
Medical history and concomitant injuries and illness.
Inhalation injury.
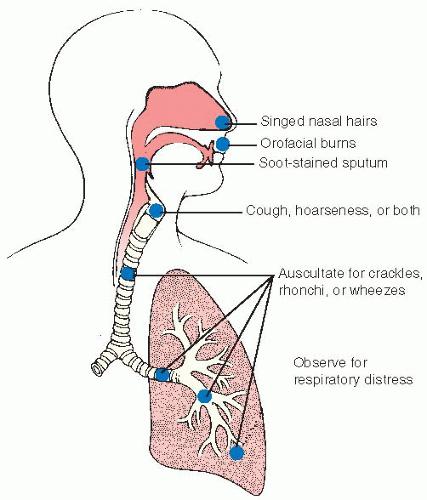
If victim was burned in a closed area, there should be a high index of suspicion that smoke inhalation has occurred.
Evaluate all patients in closed-space fires for symptoms of carbon monoxide poisoning—headache, visual changes, confusion, irritability, decreased judgment, nausea, ataxia, and collapse (see Table 34-1).
Question the patient about types of things that burned in the room—carpet, vinyl articles, and synthetics. With the increasing use of synthetics, toxicity from aldehydes, cyanide, and other substances must be considered.
Observe for upper-body burn erythema or blistering of lips, buccal mucosa, or pharynx; singed nasal hair; soot in oropharynx; dark gray or black sputum (see Figure 34-4).
Listen for hoarseness and crackles. Increasing hoarseness, stridor, and drooling are indicators of increasing need for intubation.
Obtain arterial blood gases (ABGs), carboxyhemoglobin levels, and spirometry.
Direct visualization of the vocal cords may be necessary. Further visualization may be accomplished through bronchoscopy, if necessary.
A chest x-ray should be obtained as a baseline.
Table 34-1 Signs and Symptoms of Toxicity from Carbon Monoxide | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Anatomic location—burns affecting hands, feet, face, and perineum require specialized care. Circumferential burns also require special attention, possibly escharotomy.
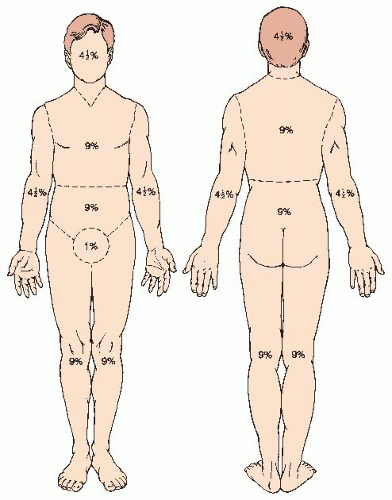
Determination is based on the use of tables for this purpose, such as the “rule of nines” (see Figure 34-5), the Lund and Browder chart (see page 1772), or the rule of the palm. The patient’s palm (including the fingers) is approximately 1% of the TBSA burned. The Lund and Browder chart is the most accurate. Calculation of the percentage of TBSA burned serves as a guide for fluid therapy. Full fluid resuscitation is necessary for partial- or full-thickness burns of 20% TBSA or greater.
Repeat assessment may be performed on the second or third day to verify demarcation of burned areas.
Table 34-2 Assessment of Burn Injury | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
It may be difficult to differentiate between second- and third-degree wounds initially. If the areas appear wet and are particularly sensate, then a second-degree (partial-thickness) injury is likely. If the area is less painful or insensate, the hairs are easily pulled out, and the area appears dry and is firm to the touch, then it is most likely a third degree (full-thickness) burn (see Table 34-2).
Reassess daily for the first few days because a partial-thickness burn can convert or progress to a full-thickness burn injury.
Deep partial-thickness burns of certain extent, full-thickness burns, chemical burns, electrical burns, burns of certain areas of the body, and any airway or inhalation injury should be transferred to a regional burn center (see Box 34-1).
 Evidence Base
Evidence Base
Partial-thickness burns of greater than 10% TBSA
Involvement of face, hands, feet, genitalia
Third-degree burns
Electrical burns
Chemical burns
Inhalation injury
Preexisting medical conditions that could complicate management
Concomitant trauma where burn injury poses greatest risk
Burned children where facilities lack qualified staff and equipment
Patients who require special social, emotional, or rehabilitative intervention