Bowel Resection With Rstomy
A bowel resection with ostomy involves the excision of diseased bowel and the creation of a stoma on the outer abdominal wall to allow elimination of feces. This surgery is performed for such intestinal maladies as inflammatory bowel disease, familial adenomatous polyposis, diverticulitis, and especially advanced colorectal cancer if conservative surgery and other treatments aren’t successful or if the patient develops acute complications, such as obstruction, abscess, or fistula.
Depending on the nature and location of the problem, the surgeon will perform one of several types of procedures. For instance, some obstructions of the ascending, transverse, descending, or sigmoid colon require a colostomy with removal of the affected bowel segments. Cancer of the rectum often mandates abdominal perineal resection, which involves wide resection of the rectum, surrounding tissues, and lymph nodes, with formation of a permanent colostomy. Perforated sigmoid diverticulitis, Hirschsprung’s disease, rectovaginal fistula, and penetrating trauma commonly call for temporary colostomy to interrupt the intestinal flow and allow healing of inflamed or injured bowel segments.
A small bowel obstruction, on the other hand, may require resection and formation of an ileostomy from the proximal ileum. Severe, widespread colonic obstruction may require total or near total removal of the colon and rectum and creation of an ileostomy. A permanent ileostomy requires that the patient wear a drainage appliance or pouch over the stoma to contain the constant fecal drainage.
Instead of a conventional stoma, patients with ulcerative colitis or familial adenomatous polyposis may be candidates for either of two surgical advances: the creation of an ileoanal reservoir or a Kock ileostomy. Both are continent diversions in which the patient retains stool until draining it. Both techniques eliminate the need to wear an external pouch or drainage bag.
Procedure
After the patient receives an anesthetic, the surgeon makes an incision in the abdominal wall. The location depends on the area of the bowel to be resected and the type of ostomy required. After excising the diseased bowel segment and, in the case of colon cancer, several more inches of bowel beyond the margins of the tumor, the surgeon creates the stoma used to drain fecal content. (See Types of intestinal stomas, page 108.)
For an abdominoperineal resection, the surgeon makes a low abdominal incision and divides the sigmoid colon. He brings the proximal end of the colon out through another, smaller abdominal incision to create an end stoma, which results in a permanent colostomy. He then makes a wide perineal incision and resects the anus, rectum, and distal portion of the sigmoid colon. He closes the abdominal wound and places one or more abdominal drains; he usually leaves the perineal wound open but may pack it with gauze or close it and place several Penrose drains.
For an ileostomy, the surgeon resects all or part of the colon and rectum (proctocolectomy). He creates a permanent ileostomy by bringing the end of the ileum out through a small abdominal incision, typically located in the right lower quadrant between the anterosuperior iliac spine and the umbilicus, and fashions a stoma.
For an ileoanal reservoir, the surgeon performs a colectomy and creates a loop or end stoma for a temporary ileostomy. He then strips the rectal mucosa to prevent recurrence of the disease, forms an internal pouch with a portion of the ileum, and performs a pouch-anal anastomosis. The temporary ileostomy is required to allow adequate healing of the internal pouch and all anastomosis sites and to allow for an increase in the capacity of the internal reservoir through fluid instillations postoperatively. It is closed after 3 to 4 months.
Types of intestinal stomas
The surgeon may construct a stoma from the large intestine in one of three ways: end, loop, or double barrel.
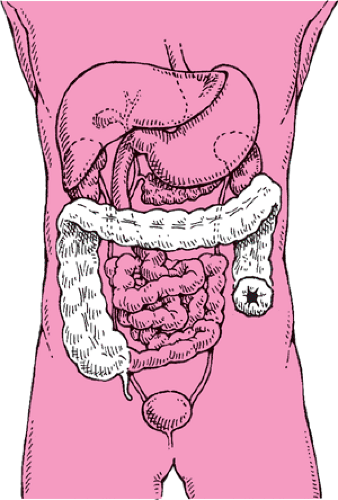
End stoma
To form an end stoma, the surgeon pulls a section of the intestine through the outer abdominal wall, everts the section, and sutures it to the skin. An ostomy with an end stoma can be either temporary or permanent.
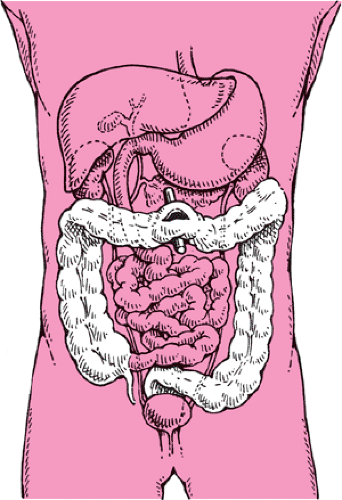
Loop stoma
To create a loop stoma, the surgeon brings a loop of intestine out through an abdominal incision to the abdominal surface and supports it with a rod or bridge (usually removed 5 to 7 days after surgery). He then opens the anterior wall of the bowel loop with a small incision to provide fecal diversion. The result is one stoma with a proximal, functioning limb and a distal, nonfunctioning limb. The surgeon then closes the wound around the exposed intestinal loop.
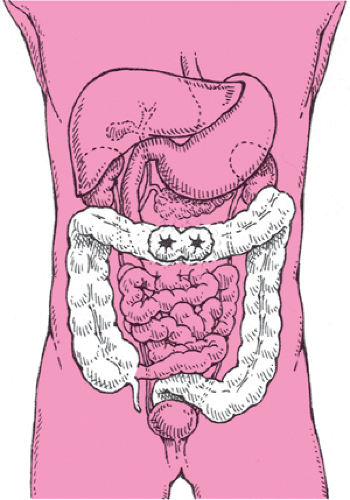
Double-barrel stoma
To create a double-barrel stoma, the surgeon divides the intestine and brings both the proximal and distal ends through the abdominal incision to the abdominal surface. He makes a small incision in the proximal stoma for fecal drainage. The distal stoma, also referred to as a mucous fistula, leads to the inactive intestine and is left intact.
Later, when the intestinal injury has healed or the inflammation has subsided, the colostomy is reversed and the divided ends of the intestine are anastomosed to restore intestinal integrity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree