Basic assessment skills
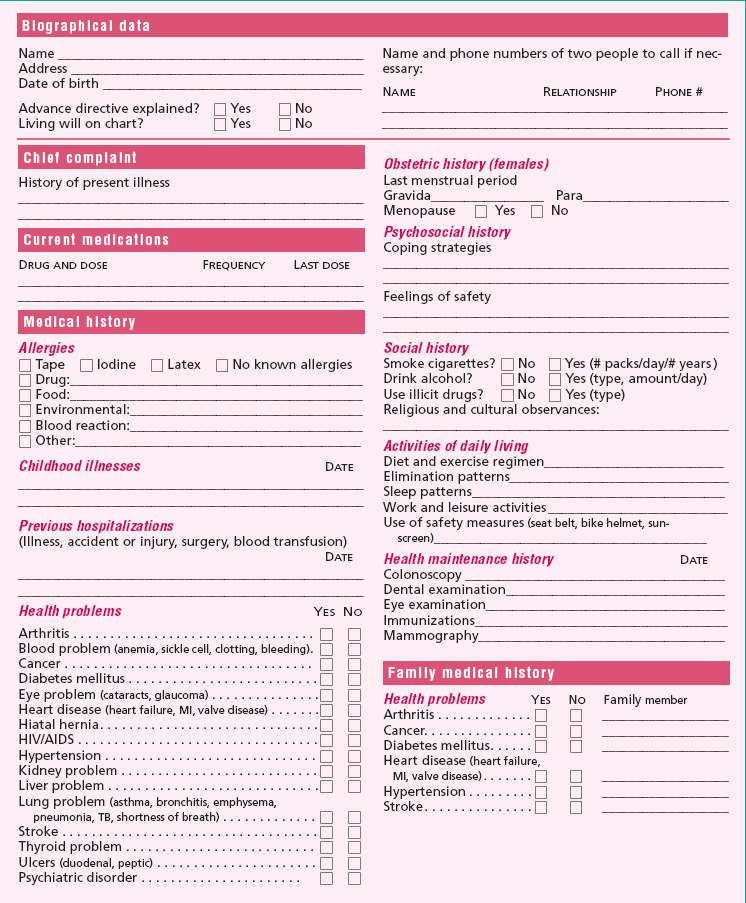
Health history
All assessments involve obtaining two kinds of data: objective and subjective. Objective data are obtained through hearing, touching, smelling, and seeing and are verifiable by someone other than the patient. For example, a red, swollen arm in a patient with arm pain is a kind of data that can be seen and verified by someone besides the patient. Subjective data can’t be verified by anyone but the patient; they’re gathered solely from the patient’s own account—for example, “My stomach hurts” or “I have trouble getting up in the morning.”
Here’s a tip to help you remember the two types of data: you observe objective data, whereas only the subject provides subjective data.
Beginning the interview
To make the most of your patient interview, create an environment in which the patient feels comfortable, and use communication strategies to make the interaction most effective.
Asking questions
Questions can be characterized as open-ended or closed.
Open-ended questions
Open-ended questions require the patient to express feelings, opinions, and ideas. They also help gather more information than can be obtained through closed questions. Open-ended questions encourage a good nurse-patient rapport because they show that you’re interested in what the patient has to say. Examples of such questions include:
Why did you come to the hospital?
How would you describe the problems you’re having with your breathing?
What lung problems, if any, do other members of your family have?
Closed questions
Closed questions elicit one- or two-word or yes-or-no responses. They limit the development of nurse-patient rapport. Closed questions can help “zoom in” on specific points, but they don’t provide the patient with an opportunity to elaborate. Examples of closed questions include:
Do you ever get short of breath?
Are you the only one in your family with lung problems?
Interviewing tips
Select a quiet, private setting.
Choose terms carefully and avoid using medical jargon. Speak slowly and clearly.
Use effective communication skills.
Use appropriate body language.
Confirm patient statements to avoid misunderstanding.
Summarize and conclude with “Is there anything else?”
Review of systems
The last part of the health history is a systematic review of each body system to make sure that important symptoms weren’t missed. The order of the review of systems is head-to-toe. This helps ensure covering all areas.
Remember when questioning an elderly patient, he may have difficulty hearing or communicating. If the patient is confused or has trouble communicating, seek assistance from a family member for some or all of the health history.
If the patient is a child, direct as many questions as possible to him. Rely on the parents for information if the child is very young.
Here are some key questions to ask the patient about each system:
Head
Do you get headaches? If so, where are they and how painful are they? How often do they occur, and how long do they last? Does anything trigger them, and how do you relieve them? Have you ever had a head injury? Do you have lumps or bumps on your head?
Eyes
When was your last eye examination? Do you wear glasses? Do you have glaucoma, cataracts, or color blindness? Does light bother your eyes? Do you have excessive tearing; blurred vision; double vision; or dry, itchy, burning, inflamed, or swollen eyes? Have you ever had eye surgery? If so, why and when?
Ears
Do you have loss of balance, ringing in your ears, deafness, or poor hearing? Have you ever had ear surgery? If so, why and when? Do you wear a hearing aid? Are you having pain, swelling, or discharge from your ears? If so, has this problem occurred before, and how frequently?
Nose
Have you ever had nasal surgery? If so, why and when? Have you ever had sinusitis or nosebleeds? Do you have nasal problems that impair your ability to smell or that cause breathing difficulties, frequent sneezing, or discharge?
Mouth and throat
Do you have mouth sores, dry mouth, loss of taste, toothache, or bleeding gums? Do you wear dentures and, if so, do they fit? Do you have a sore throat, fever, or chills? How often do you get a sore throat, and have you seen a doctor for this?
Do you have difficulty swallowing? If so, is the problem with solids or liquids? Is it a constant problem or does it accompany a sore throat or another problem? What, if anything, makes it go away?
Neck
Do you have swelling, soreness, lack of movement, stiffness, or pain in your neck? If so, did something specific cause it to happen? How long have you had this symptom? Does anything relieve it or aggravate it?
Skin, hair, and nails
Do you presently have any skin disorders, such as psoriasis? Do you have any rashes, scars, sores, ulcers, or areas with abnormal skin color? Do you have skin growths, such as warts, moles, tumors, or masses? Do you experience skin reactions to hot or cold weather? Have you noticed changes to the amount, texture, or character of your hair? Have you noticed changes in your nails? Do you experience excessive nail splitting, cracking, or breaking?
Respiratory system
Do you ever have shortness of breath? Does anything relieve it or aggravate it? How many pillows do you use at night? Does breathing cause pain or wheezing? Do you have a productive cough? If so, describe the sputum. Do you have night sweats?
Have you ever been treated for pneumonia, asthma, emphysema, or frequent respiratory tract infections? Have you ever had a chest X-ray or tuberculin skin test? If so, when, and what were the results?
Cardiovascular system
Do you ever have chest pain, palpitations, irregular heartbeat, fast heartbeat, shortness of breath, or a persistent cough? If so, what aggravates it or relieves it? Have you ever had an electrocardiogram? If so, when, and what were the results?
Do you have high blood pressure, peripheral vascular disease, swelling of the ankles and hands, varicose veins, cold extremities, or intermittent pain in your legs? Have you experienced dizziness or fainting?
Breast and axilla
Ask women: Do you perform monthly breast self-examinations? Have you noticed a lump, a change in breast contour, breast pain, or discharge from your nipples? Have you ever had breast cancer? If not, has anyone else in your family had it? Have you ever had a mammogram? When, and what were the results?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access