Asthma
Description
Chronic reactive airway disorder that involves episodic, reversible airway obstruction, resulting from bronchospasm, increased mucus secretions, and mucosal edema
Signs and symptoms ranging from mild wheezing and dyspnea to life-threatening respiratory failure
Signs and symptoms of bronchial airway obstruction possibly persisting between acute episodes
May occur at any age; about 50% of all patients with asthma under age 10, affecting twice as many boys as girls
In about one-third of patients, onset between ages 10 and 30
Disease shared with at least one immediate family member in about one-third of cases
Intrinsic and extrinsic asthma possibly coexisting in many asthmatics
Pathophysiology
Tracheal and bronchial linings overreact to various stimuli, causing episodic smooth-muscle spasms that severely constrict the airways.
Mucosal edema and thickened secretions further block the airways.
Immunoglobulin (Ig) E antibodies, attached to histamine-containing mast cells and receptors on cell membranes, initiate intrinsic asthma attacks.
When exposed to an antigen such as pollen, the IgE antibody combines with the antigen. (On subsequent exposure to the antigen, mast cells degranulate and release mediators.)
Mediators cause bronchoconstriction and edema of an asthma attack.
During an asthma attack, expiratory airflow decreases, trapping gas in the airways and causing alveolar hyperinflation.
Atelectasis may develop in some lung regions.
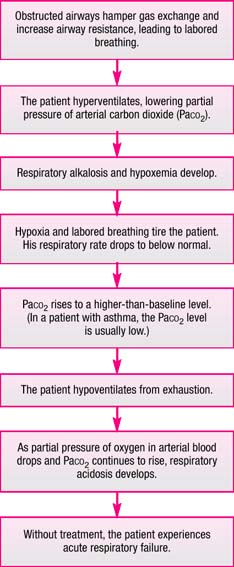
Increased airway resistance initiates labored breathing. (See What happens in status asthmaticus, page 24.)
Causes
Sensitivity to specific external allergens or from internal, nonallergenic factors
Bronchoconstriction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree