Arthritis
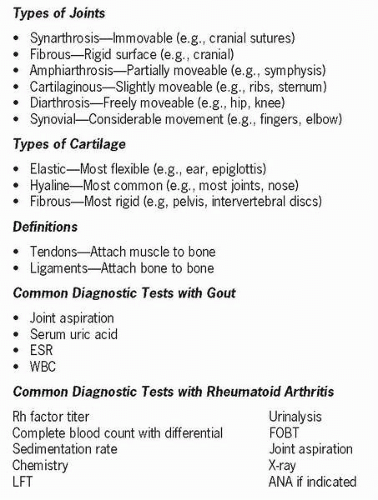
Arthritis, a term applied to many different conditions, is the second leading cause of disability in the United States. Arthritis is the inflammation of a joint that can manifest as many different forms. Some forms are due to disease or trauma, whereas others are related to infections and metabolic or autoimmune disorders. Three major forms of arthritis include osteoarthritis, rheumatoid arthritis (RA), and gout. All three of these diseases involve the entire joint structure, including the synovial membrane, articular cartilage, tendons, ligaments, adjacent bone, and joint spaces. X-ray is used to confirm diagnosis and monitor progression. Specific laboratory tests are available for rheumatoid or autoimmune forms.
Osteoarthritis is a progressive degenerative joint disease affecting primarily peripheral and central weight-bearing joints and fingers and is the most common form of arthritis in adults and elderly. The hallmark of this disease is progressive loss of articulating cartilage. Primary or idiopathic osteoarthritis is associated with aging, whereas secondary osteoarthritis is related to some other condition or
process and is often a result of repeated or severe joint stress or trauma. Osteoarthritis has an asymmetrical distribution and is a local disease. Degenerative changes often begin between the ages of 40 and 50. Early symptoms are often mild and frequently ignored or compensated for by those who have them. The incidence is higher in males.
process and is often a result of repeated or severe joint stress or trauma. Osteoarthritis has an asymmetrical distribution and is a local disease. Degenerative changes often begin between the ages of 40 and 50. Early symptoms are often mild and frequently ignored or compensated for by those who have them. The incidence is higher in males.
Collagen is the primary building block of cartilage. It is continuously being renewed and remodeled by chondrocytes. Cartilage does not possess a blood supply or nerve endings; therefore, it requires long periods of time to heal. It is nourished by diffusion of nutrients from surrounding capillaries. Its function is to absorb shock, reduce friction, and distribute weight bearing. Tendons have pain receptors but a limited blood supply, so they also take a long time to heal. Joint spaces are filled with synovial fluid, which lubricates, nourishes, cushions, and facilitates movement.
Pathophysiology
Osteoarthritis is characterized by progressive erosion of articular cartilage, which results from the breakdown of protein and collagen by enzymes. Increased water is absorbed because of disruption in pumping action, so the cartilage becomes less able to tolerate weight bearing and loses some of its tensile strength. As osteoarthritis progresses, bits of articular cartilage flake off and longitudinal fissures develop. The cartilage becomes thin or absent, leaving the bone unprotected. Subchondral bone thickens and becomes sclerotic with potential of cyst formation. Osteophytes (bone spurs) develop at the joint margin, which can also break off, causing synovitis and joint effusion. The joint capsule becomes thickened and may adhere to underlying structures. Knees, hips, vertebrae, and fingers are the most common sites. Pain associated with osteoarthritis arises from a combination of articular distension, inflammation, and fibrosis.
Management
Osteoarthritis is managed by a combination of rest and exercise, including range of motion exercises to maintain joint mobility. Weight reduction is important if indicated. Ambulation aids may be necessary to reduce stress on weight-bearing joints. Pain management with acetaminophen and other nonsteroidal antiinflammatory drugs (NSAIDs) is the mainstay of therapy. Cyclooxygenase-2 inhibitors are used sparingly and in those patients without risk of vessel disease or bleeding abnormalities. Patient education is important in the management of this chronic condition. Surgery and joint replacement is sometimes indicated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree