Arrhythmias
Arrhythmias result from abnormal electrical conduction or automaticity that changes heart rate and rhythm. They vary in severity, from those that are mild, asymptomatic, and require no treatment (such as sinus arrhythmia, in which heart rate increases and decreases with respiration) to catastrophic ventricular fibrillation, which requires immediate intervention.
Arrhythmias are classified according to their origin as ventricular, atrial (supraventricular), or junctional. Their effect on cardiac output and blood pressure, partially influenced by the site of origin, determines their clinical significance.
Causes
Arrhythmias may be congenital or may result from myocardial ischemia or infarction, organic heart disease, drug toxicity, or degeneration of conductive tissue necessary to maintain normal heart rhythm (sick sinus syndrome).
Complications
In a patient with a normal heart, arrhythmias typically produce few symptoms. But even in a normal heart, persistently rapid or highly irregular rhythms can strain the myocardium and impair cardiac output.
Assessment
Depending on the arrhythmia, the patient may exhibit symptoms ranging from pallor, cold and clammy extremities, reduced urine output, palpitations, and weakness to chest pains, dizziness and, if cerebral circulation is severely impaired, syncope.
Diagnostic tests
Electrocardiography (ECG) allows detection and identification of arrhythmias. (See Types of cardiac arrhythmias.)
Treatment
Effective treatment aims to return pacer function to the sinus node, increase or decrease ventricular rate to normal, regain atrioventricular synchrony, and maintain normal sinus rhythm. Such treatment corrects abnormal rhythms through therapy with antiarrhythmic drugs; electrical conversion with precordial shock (defibrillation and cardioversion); physical maneuvers, such as carotid massage and Valsalva’s maneuver; temporary or permanent placement of a pacemaker to maintain heart rate; implantable cardioverter defibrillation if indicated; and surgical removal or cryotherapy of an irritable ectopic focus to prevent recurring arrhythmias. Indications for ablation therapy are atrial fibrillation or ventricular tachycardia that doesn’t respond to other therapies.
Arrhythmias may respond to treatment of the underlying disorder such as correction of hypoxia. However, arrhythmias associated with heart disease may require continuing and complex treatment.
Key nursing diagnoses and patient outcomes
Ineffective tissue perfusion (cerebral) related to decreased cardiac output from an arrhythmia. Based on this nursing diagnosis, you’ll establish these patient outcomes. The patient will:
not develop complications caused by ineffective cerebral tissue perfusion, such as stroke or seizures
maintain adequate cerebral perfusion, as evidenced by being oriented to time, person, and place
maintain hemodynamic stability.
Anxiety related to potential for arrhythmia to become life-threatening. Based on this nursing diagnosis, you’ll establish these patient outcomes. The patient will:
express feelings of anxiety
use support systems to assist with coping
experience diminished physical symptoms of anxiety.
Decreased cardiac output related to decreased left ventricular filling time caused by the arrhythmia. Based on this nursing diagnosis, you’ll establish these patient outcomes. The patient will:
not exhibit signs of decreased cardiac output, such as hypotension and ineffective tissue perfusion
recover a normal cardiac rhythm that will remain normal
communicate understanding of medical therapy to treat and prevent arrhythmias.
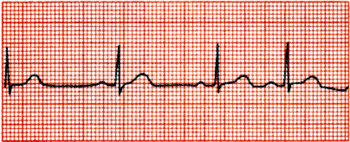
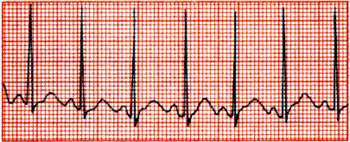
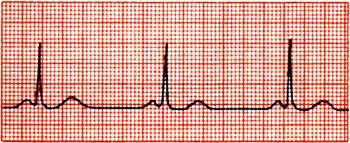
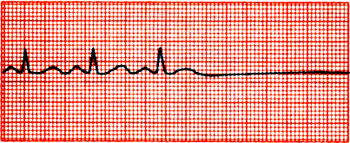
Types of cardiac arrhythmias
This chart reviews several common cardiac arrhythmias and outlines their characteristics, causes, and treatments. For comparison, here’s a normal cardiac rhythm strip and its characteristics.
Ventricular and atrial rates 60 to 100 beats/minute
Regular and uniform QRS complexes and P waves
PR interval of 0.12 to 0.2 second
QRS duration < 0.12 second
Identical atrial and ventricular rates, with constant PR interval
|