Acid-Base Balance
Maintenance of acid-base balance is critical for life and health and is achieved through various buffer systems and compensatory mechanisms of the lungs and kidneys. These imbalances can range from mild to severe and life threatening, and there is a narrow therapeutic window. Regulation of the pH is due to the concentration of hydrogen in the blood. When there are changes in the concentration of this ion, imbalances occur.
TERMS
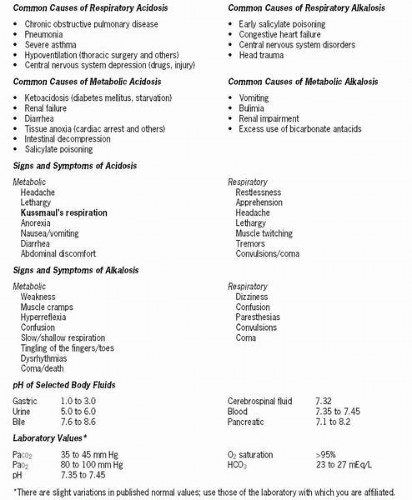 Figure 4-1 Common causes of respiratory acidosis. |
Hydrogen ions maintain membrane integrity and speed of enzymatic reactions. Their concentration is expressed as pH. When there is a higher number of hydrogen ions, the solution is more acidic, which lowers pH. Conversely, when there is a lower number of hydrogen ions, the solution is more basic, which raises the pH. Acids are produced as a byproduct when protein, carbohydrate, and fat metabolize.
The respiratory and renal systems have primary responsibility for maintaining pH within a normal range. The lungs excrete volatile acids (carbonic acid) by eliminating carbon dioxide (CO2), whereas the kidneys excrete nonvolatile acids such as sulfuric, phosphoric, and organic by regulating bicarbonate. Buffer systems assist in this process.
Buffer Systems
Buffers absorb excess acid (H+) or excess base (OH−) without a significant change in pH. They work as pairs, each containing a weak acid and a weak base. The carbonic acid-bicarbonate buffer system is the most important extracellular buffer system. Hemoglobin is an important buffer in erythrocytes. Phosphorus and protein are the primary intracellular buffers. Most buffer systems disassociate rapidly in response to changes in pH. The carbonic acid-bicarbonate buffer system acts in both the lungs and the kidneys. As the PaCO2 increases in the blood, more carbonic acid is formed. The lungs compensate for this by blowing off CO2, and the kidneys compensate by either reabsorbing bicarbonate or producing more. The respiratory response
begins within minutes or hours. The renal response occurs within hours or days. Conversely, if the ratio between bicarbonate (HCO3) and carbonic acid (H2CO3) shifts toward the basic side, H+ is conserved or produced by the kidneys and the lungs retain CO2 (allowing more carbonic acid to be formed). The lungs respond similarly to changes in nonvolatile acid levels, which compensates for it. This response takes a little longer. When the body is adequately compensating for changes in pH, the pH of the blood is normal but there are variations in the levels of HCO3 or PaCO2 and other blood chemistry values. This compensation may also be reflected in changes in respiratory rate and depth and pH of the urine. The elderly respond less quickly to changes in pH.
begins within minutes or hours. The renal response occurs within hours or days. Conversely, if the ratio between bicarbonate (HCO3) and carbonic acid (H2CO3) shifts toward the basic side, H+ is conserved or produced by the kidneys and the lungs retain CO2 (allowing more carbonic acid to be formed). The lungs respond similarly to changes in nonvolatile acid levels, which compensates for it. This response takes a little longer. When the body is adequately compensating for changes in pH, the pH of the blood is normal but there are variations in the levels of HCO3 or PaCO2 and other blood chemistry values. This compensation may also be reflected in changes in respiratory rate and depth and pH of the urine. The elderly respond less quickly to changes in pH.
 The lungs compensate for this increase in carbonic acid by blowing off CO2, and the kidneys compensate by either reabsorbing bicarbonate or producing more.
The lungs compensate for this increase in carbonic acid by blowing off CO2, and the kidneys compensate by either reabsorbing bicarbonate or producing more.Proteins carry negative charges and are buffers for H+. Hemoglobin is an excellent intracellular buffer because it binds readily with H+ and CO2. In addition, the kidney regulates amounts of PO4 and ammonia in response to changes in the pH of the blood, which allows H+ to be excreted in the urine. These systems work in conjunction with the H+ ion and bicarbonate renal mechanisms previously described to effect a normal pH and maintain homeostasis. Shifts in K+ and H+ ions in acidosis or alkalosis also assist in buffering. In acidosis, H+ cannot be excreted without another cation being retained. Because K+ is the ion retained, hyperkalemia develops in acidosis. Additionally, when excess H+ moves into the cell, K+ leaves, further contributing to hyperkalemia. The reverse happens with alkalosis, resulting in hypokalemia. Ca++ is also affected by serum pH. More Ca++ is bound with serum proteins in an alkalotic state; therefore hypocalcemia accompanies alkalosis, and hypercalcemia accompanies acidosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






